- How many reasons can you cite to support a diagnosis of VT (Ventricular Tachycardia)?
.jpg) |
| Figure 1: 12-lead ECG from a patient whose BP was dropping. |
==========================
NOTE: Because of the length of this Blog — We offer all Tables and Figures at this LINK (on Blog 42-bis) — so as to facilitate side-by-side viewing. Tables/Figures are also found here at the bottom.
==========================
NOTE: Because of the length of this Blog — We offer all Tables and Figures at this LINK (on Blog 42-bis) — so as to facilitate side-by-side viewing. Tables/Figures are also found here at the bottom.
==========================
ANSWER to Figure 1:
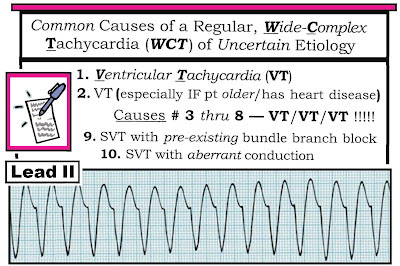
The 12-lead ECG in the Figure shows a regular WCT (Wide Complex Tachycardia)
rhythm at a rate of ~180/minute. Sinus P waves are absent. The rhythm is sustained
VT — and the patient is in need of immediate electrical therapy (synchronized
cardioversion or defibrillation). Many reasons can be cited to support
definitive diagnosis of sustained VT. These include:
1) Statistically — at least 80% of all regular
WCT rhythms of uncertain etiology are VT. The likelihood of VT increases to over
90% IF the patient is middle-aged or older — and especially if the patient has
underlying heart disease.
- Although on occasion regular WCT rhythms may be due to a supraventricular etiology with either preexisting bundle branch block or aberrant conduction — VT must always be assumed until proven otherwise (See Table 1 below or at 42-bis). In addition to being so much more common than wide-QRS complex SVT rhythms — VT is a potentially life-threatening arrhythmia.
2) Extreme axis deviation is present. Mild-to-moderate
left or right axis deviation may be seen with supraventricular rhythms.
However, total negativity in either lead I or lead aVF suggests extreme axis
deviation, and is almost of itself diagnostic of VT.
3) The QRS complex is both markedly widened (to
over 0.16 second in many leads) — and — the QRS is lacking in organized morphology
(which we convey by describing QRS appearance as “ugly”…). Both features are
highly suggestive of VT. Aberrant conduction most often manifests a more
organized QRS morphology that is consistent with some type of conduction defect
(left or right bundle branch block with or without hemiblock).
4) There is ECG evidence of delayed initial ventricular
activation. The presence of an r-to-S-nadir of more than 0.10 second in one or
more precordial leads is highly suggestive of VT. This is best seen in lead V5.
5) One should always assume VT until proven
otherwise. The patient should be treated accordingly.
==========================
KEY Clinical Principles to Apply for the
Patient in WCT:
Many ECG criteria have been cited to assist in
assessment of WCT rhythms. We extensively review this topic elsewhere (See link to Sections 08.0,09.0 in the References below). For the purposes of this ECG Blog #42 — We consolidate
key principles as they apply to the ECG and clinical scenario presented in Figure
1.
==========================
Our Suggested Approach to the patient in a WCT
rhythm is as follows:
- First determine IF the patient is hemodynamically stable. IF the patient is unstable — it no longer matters what the rhythm is, since immediate electrical therapy (synchronized cardioversion or defibrillation) is indicated.
- IF the patient with tachycardia is initially stable — BUT at any time becomes unstable — electrical therapy is then immediately indicated.
- IF the rhythm diagnosis is known to be VT — treat accordingly (See link to Section 07.0 in the References below).
- IF the rhythm diagnosis of the WCT rhythm is known to be SVT — then a different approach should be followed, depending on our “best guess” as to the etiology of the SVT (See ECG Blog #40 and the link to Section 13.0 in the References below).
- Special considerations and treatment interventions are warranted for the patient with stable but irregular WCT — given the possibility of Torsades de Pointes, polymorphic VT, and very rapid AFib with WPW (See ECG Blog #36).
- But IF the patient is stable — and — the rhythm is a regular WCT of uncertain etiology — then focused attention to a few selected ECG Features can greatly increase the certainty of our presumed diagnosis.
==========================
Which ECG Criteria to Use for Assessing WCT
Rhythms?
Many criteria exist for assessing WCT rhythms.
We list below our preference for those criteria we feel are: i) easy-to-use and
remember; and ii) very useful clinically:
- We start with 3 Simple Rules (Table 2). In our experience — these 3 user-friendly Rules are all that is needed for near definitive diagnosis of VT in most cases.
- RULE #1: Is there extreme axis deviation? IF so — then VT is highly likely. We emphasize that mild or even moderate left or right axis deviation (LAD or RAD) does not assist in distinguishing between VT and SVT. But — when there is extreme axis deviation (as seen for the marked RAD in Figure 1 — in which the QRS complex in lead I is entirely negative) — then the chance of VT is greatly increased. NOTE: The "quick way" to recognize that there is "extreme" axis deviation — is if the QRS complex is entirely negative in either lead I or in lead aVF. And while exceptions exist (ie, some patients with severe heart disease may have extremely abnormal baseline tracings — and some patients with LBBB may manifest an all negative QRS in lead aVF as part of their LBBB) — recognition of "extreme" axis deviation is EASY to do, and often provides invaluable information.
- RULE #2: Look at QRS morphology in Lead V6. When the etiology of the rhythm is supraventricular — there will almost always be at least some positive activity traveling toward the LV (and therefore positive in lead V6). IF ever the QRS complex in lead V6 is either all negative or almost all negative — then VT is highly likely. We emphasize that lead V6 is only helpful when it is predominantly negative. Thus, the positive R wave we see in lead V6 of Figure 1 is not diagnostic (See Figure 2).
- RULE #3: The “uglier” the QRS complex during the WCT rhythm — the more likely the rhythm is VT. The reason for this is that aberrant conduction almost always manifests some form of conduction defect (RBBB, LBBB, LAHB, LPHB – or some combination thereof) — due to relative delay in one or more of the hemifascicles or bundle branches. In contrast — VT originates from a ventricular focus outside of the conduction system (and is therefore more likely to be wider and far less organized in its conduction pattern). The QRS complex in Figure 1 is extremely wide (over 0.16 second) and formless. This makes supraventricular conduction much less likely.
- Is there AV Dissociation during the WCT rhythm? IF so — this is virtually diagnostic of VT. That said — most of the time, AV dissociation will not be seen unless the rate of VT is relatively slow. Therefore — the absence of AV dissociation is nondiagnostic. However, its presence may be confirmatory. Although it is possible that 1:1 retrograde atrial conduction may be seen in Figure 1 (in the form of subtle notching in the ST-T wave of lead II and in lateral precordial leads) — normal sinus P waves are clearly absent. Thus, there is no indication of AV dissociation. (For more on AV Dissociation with VT — See ECG Blog #133).
- Is there concordance of the QRS complex in all precordial leads? IF ever all QRS complexes in leads V1-thru-V6 are either all positive or all negative — this is virtually diagnostic of VT. That said — the sensitivity of this finding is extremely low, such that the lack of precordial lead concordance is not at all helpful. Concordance is not present in Figure 1 — because the QRS is clearly positive in lead V6.
- Is the R-to-S nadir in any precordial lead delayed to >0.10 second? Brugada’s 2nd criterion for assessing WCT rhythms (and Sasaki’s 2nd criterion) specify delay in attaining the R-to-S nadir in any precordial lead as highly suggestive of VT (See Figure 3). If no delay is seen in attaining R-to-S nadir — then nothing can be said. The physiologic rationale for the R-to-S nadir delay criterion is that the initial path of supraventricular impulses is usually conducted with no more than minimal delay.
- Most regular WCT rhythms will manifest an RS complex in at least one precordial lead (IF there is no RS complex in any precordial lead – then by Brugada’s 1st criterion the rhythm is VT!). The main caveat to be aware of is that the boundaries of QRS onset and S wave nadir are not always clear. However — R-to-S nadir in lead V5 of Figure 1 appears to definitely exceed 0.10 second in duration.
- Is there a tall monophasic R wave in lead aVR? With normal sinus rhythm — lead aVR manifests a predominantly negative QRS complex. This reflects the normal path of ventricular activation — which moves away from the right (away from aVR) — and toward the left ventricle. IF ever the QRS complex in lead aVR during WCT is entirely positive — this means that the electrical impulse must be originating from a site in the ventricular apex and traveling upward toward the base (in the direction of aVR). Thus, a quick look at lead aVR during a WCT rhythm can sometimes tell you (with virtual 100% specificity) that the rhythm is VT (See Figure 4). That said — this criterion is relatively insensitive, such that most of time QRS appearance in lead aVR will be nondiagnostic. Lead aVR is nondiagnostic in Figure 1.
- Is QRS morphology typical of aberrant conduction? For practical purposes — the only QRS morphology form with high specificity for SVT is the presence of typical RBBB. By far the best lead to recognize this in is lead V1 (See Figure 2 below). Thus, the presence of an rsR’ complex (with ‘taller-right-rabbit-ear’ and S wave that descends below the baseline) — strongly suggests a supraventricular etiology (A,B in Fig. 2). In contrast — any other QRS morphology in lead V1 (C,D,E,F) serves to increase the likelihood of VT. This includes an upright, widened QRS with a notch that does not descend below the baseline (C) – as well as a monophasic R without any notch (D) — a qR pattern (E) — and/or a taller left rabbit ear with or without a notch (F).
- Assessment of QRS morphology in Figure 1 — clearly does not resemble typical RBBB (instead the QRS is entirely negative in lead V1). As already noted — QRS morphology in Figure 1 is “ugly” (formless) — not suggestive of either typical LBBB or RBBB — and therefore strongly in favor of VT as the etiology.
- NOTE: For there to be "typical RBBB morphology" — in addition to the above described rsR' complex, there should also be wide terminal S waves in leads I and V6. Without these findings in all 3 of the key leads (ie, leads I, V1, V6) — there is not a "typical" RBBB pattern, and the specificity for distinction between VT vs SVT is lost.
- Clinical Parameters: While exceptions definitely occur — the fact that a patient is “younger” and previously healthy prior to the arrhythmia episode does make an ischemic form of VT much less likely. In contrast, even before looking at specific ECG features — IF the patient presenting with a regular WCT of uncertain etiology is “older” and has a history of significant heart disease — then then statistical likelihood of VT approaches 90%.
==========================
NOTES regarding Clinical Parameters:
- Is the patient “older” ? While there are no specific age “cutoffs” for what is ‘older’ or ‘younger’ — a patient in their 20’s, 30’s or early 40’s is relatively more likely to have SVT than a patient older than 55. This is especially true IF this younger adult was previously healthy with no known underlying heart disease.
- A select group of VT rhythms (as many as 5-10% of all VT rhythms) — may respond to Adenosine! While certain ECG characteristics may suggest an adenosine-responsive form of VT (See ECG Blog #35) — ECG recognition of adenosine-responsive VT will not always be possible. Awareness of this clinical reality provides a rationale for trial of empiric Adenosine at an early point in the treatment approach to monomorphic regular WCT.
- Adenosine-responsive forms of VT — are much more likely to occur in younger adults without underlying heart disease. They often occur during exercise — and the patient will often remain hemodynamically stable during the WCT rhythm. Thus, even IF a previously healthy young adult presents with VT — the chances are surprisingly good that the rhythm will respond to Adenosine. That said — the above discussion does not apply to the case in Figure 1, because the patient was unstable and in need of immediate cardioversion. (For more on VT in patients without underlying heart disease = Idiopathic VT — See ECG Blog #197).
==========================
SUMMARY:
Always think, “VT until proven otherwise” —
whenever you encounter a patient in a regular WCT rhythm of uncertain etiology.
Treatment will depend on hemodynamic stability and clinical parameters. Our
hope is that review of this ECG Blog #42 will increase your comfort in the relative
certainty of your rhythm diagnosis.
-==========================
==========================
Supportive Tables and Figures for this ECG
Blog #42 (also found at 42-bis):
- Included below are key visuals we refer to in this ECG Blog #42 for assisting in differentiation of WCT rhythms (Please also see links to Sections 08.0,09.0 in the References below):
==========================
 |
| Table 2: After applying Table 1 (ie, "Assume VT until until proven otherwise) — we move to the 3 Simple Rules — which in our experience is often all that is needed for near-definitive diagnosis. |
==========================
==========================
==========================
Figure 4: The presence of a large upright R
wave in lead aVR during a WCT rhythm is virtually diagnostic of VT (since this
finding implies ventricular activation begins in the apex). Finding a QR
complex or a small amplitude complex (2nd and 3rd examples shown) is
nondiagnostic.
==========================
Selected REFERENCES:
- Brugada P, Brugada J, Mont L, et al: A New Approach to the Differential Diagnosis of a Regular Tachycardia with a Wide QRS Complex. Circulation 83:1649-1659, 1991.
- Blomstrom-Lundqvist C, Scheinman MM, Aliot EM, et al: ACC/AHA/ESC Guidelines for Management of Patients with Supraventricular Arrhythmias — Executive Summary. J Am Coll Cardiol 42:1493-1531, 2003.
- Vereckei A, Duray G, Szenasi G: Application of a New Algorithm in the Differential Diagnosis of Wide QRS Complex Tachycardia. Eur Heart J 28:589-600, 2007.
- Sasaki K: A New Simple Algorithm for Diagnosing Wide QRS Complex Tachycardia: Comparison with Brugada, Vereckei and aVR Algorithms. Circulation 120:S671, 2009.
- Chen et al: A New, Simple ECG Algorithm for Rapid Identification of VT based on Opposing QRS Complexes (OQL) on Limb Leads. JACC 73:9:319, 2019 — CLICK HERE for Figure illustrating application of OQL. (NOTE: The OQL criteria is a little more specific than my above "extreme axis deviation" criteria. I do not know if OQL is necessarily better than my criterion .... but as it is new and potentially more specific — I'm adding this reference [10/5/2019]).
- These same authors (Chen et al) then combine #1) OQL — and/or — #2) Monophasic R in aVR — and/or — #3) A predominantly negative QRS in leads I,II,III — for which #3) is easy-to-assess and different from my criteria, so worth considering! — Chen et al: Simple ECG Criteria for Rapid ID of Wide QRS Tachy: the New Limb Lead Algorithm (LLA) — ON LINE LINK —
==========================
— Back to ECG BLOG #42-Bis —
==========================
- Section 06.0 — on Using Adenosine -
- Section 07.0 — on Known VT -
- Sections 08.0, 09.0,10.0 — on the regular Wide Tachycardia
- Section 13.0 — on SVT of Uncertain Etiology -
-----------------------------------------------------------------------

.jpg)
.jpg)
.jpg)
Very nice practical review of wide QRS tachycardia sir. From a different perspective ("floor people") , we see those things initially with 1 lead( II or V1) then open the 7 or 8 channel (limb leads and V1). With 1 lead I check AV dissociation but in reality it is really hard. Then I go for V1 (LBBB morphology). I will right away lean towards VT with the RS interval at 120 ms and the notching of the downstroke. Thanks for reminding the axis.
ReplyDeleteThis comment has been removed by the author.
DeleteTHANK YOU for your kind words. Please also check out ACLS Comments- ISSUE #11 (at: https://www.kg-ekgpress.com/acls_comments-_issue_11/ ) - which reviews the topic of VT vs aberrant conduction in even more detail in full interactive format. - Ken Grauer, MD
DeleteThank you very much for the extremely valuable information Dr,Ken Grauer
ReplyDeleteVery helpful. Thank you.
ReplyDeleteGreat presentation. Valuable information!
ReplyDelete