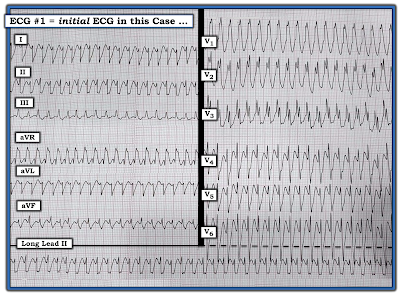
- How would YOU interpret this ECG?
- Why are there 3 different QRS shapes?
- Has there been a recent infarction?
- Does the Ashman Phenomenon apply?
My Sequential Thoughts for Interpreting this Tracing:
As always — I began my systematic approach with assessment of the rhythm. This is especially important to do for today's tracing — because it is all but impossible to interpret the 12-lead ECG in Figure-1 without full awareness of what is going on with the rhythm!
- PEARL #1: It is often insightful to spend a few seconds (No more than 5 seconds should be needed!) — by stepping back, and taking a look at the overall pattern of the rhythm (if there is one). In Figure-1 — I was struck by the repetitive pattern of 3-beat groups that preserved the identical sequence of changing morphologies with a very similar sequence of R-R intervals throughout the tracing. This could not be by chance!
I next began my systematic approach to the rhythm in my usual manner, with assessment of the Ps, Qs and 3Rs (as discussed in detail in ECG Blog #185).
- NOTE: It does not matter in what sequence you assess the 5 parameters in the Ps, Qs, 3R Approach — as long as you always look for each of these 5 parameters with every rhythm you encounter (ie, Look for P waves — QRS width — Rate and Regularity of the rhythm — and whether P waves are Related to neighboring QRS complexes). I'll often vary the sequence I choose — depending on particulars of the rhythm at hand.
- In Figure-1 — we've already looked at Regularity of the rhythm, for which we noted in PEARL #1 the repetitive pattern of 3-beat groups.
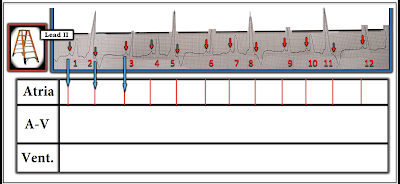
- PEARL #2: I've often been amazed at how helpful the simple step to label P waves can be for clarifying the mechanism of the rhythm. Complex relationships between P waves and neighboring QRS complexes often become obvious once this simple step is done. Along the way — I like to number the beats, which greatly facilitates your communication when discussing the rhythm with colleagues (Figure-2).
 |
| Figure-2: I've labeled the P waves that can clearly be seen (See text). |
- Do YOU see any indication in Figure-2 that there might be more P waves than the ones that I labeled?
- KEY Point: Where is the best place to look for additional P waves?
- IF an underlying sinus rhythm is present — the best place to look for additional P waves in Figure-2, will be approximately midway between each of the longer spaces on the rhythm strip in which there are no RED arrow P waves.
- Using calipers facilitates process!
- What do you see in Figure-3?
- The underlying mechanism of the rhythm is sinus. PINK arrows reveal that P waves were "hiding" just after the QRS complex of beats #2, 5, 8 and 11.
- The P-P interval does vary a little throughout this rhythm strip. This is consistent with sinus arrhythmia.
- The PR interval is constant and normal (ie, ≤0.20 second) before beats #3, 6, 9 and 12. The QRS complex of each of these beats is narrow. Therefore — the 1st beat in each of the 3-beat groups (ie, beats #3, 6, 9 and 12) is sinus-conducted.
- Although the QRS complex of the 2nd beat in each group is wide — the PR interval preceding these beats (ie, beats #4, 7 and 10) is the same as the PR interval preceding beats #3, 6, 9 and 12. Therefore — beats #4, 7 and 10 (and also beat #1 at the beginning of the tracing) — are all sinus-conducted, but with bundle branch block!
- Beats #2, 5, 8 and 11 are wide and very different in shape from the other wide beats in this tracing. These beats occur early, and are not preceded by a premature P wave. Therefore — beats #2, 5, 8 and 11 are PVCs (Premature Ventricular Contractions).
- PEARL #3: Some PVCs conduct retrograde to the atria. Some do not. The fact that sinus P waves continue throughout the long lead II rhythm strip in Figure-3 without being inhibited by wide beats #2, 5, 8 and 11 proves that these wide beats are PVCs. This is because IF these beats were either aberrantly conducted PACs or PJCs — they would have "reset" the SA Node, which would have suppressed the PINK arrow sinus P waves.
- P waves — The PINK and RED arrows show fairly regular sinus P waves, consistent with sinus arrhythmia.
- QRS width — Sinus-conducted beats #3, 6, 9 and 12 are narrow. Sinus-conducted beats #1, 4, 7 and 10 are wide and conduct with bundle branch block.
- Regularity — There is a repetitive pattern to the rhythm, with similar looking 3-beat groups.
- Rate — The P-P interval between any 2 consecutive RED arrows is between 3-to-4 large boxes, corresponding to an underlying atrial rate of ~85/minute.
- Related — The PR interval preceding the first 2 beats in each group is constant, such that these P waves are related to neighboring QRS complexes (ie, these beats are sinus-conducted).
- PEARL #4: I believe the reason beats #1, 4, 7 and 10 all conduct with BBB aberration — is that this represents an unusual manifestation of the Ashman Phenomenon. Simply stated — the Ashman Phenomenon results from the fact that the RP (Refractory Period) is in large part determined by the duration of the preceding R-R interval. The longer the preceding R-R interval — the longer the subsequent RP — and the greater the chance that an earlier beat will encounter a part of the conduction system that is still in a refractory state (ie, "The funniest-looking beat follows the longest pause"). In Figure-3 — beats #4, 7 and 10 all follow the longest pauses in this tracing, which therefore accounts for the BBB aberration.
- Beyond-the-Core: QRS morphology for aberrantly-conducted beats #1, 4, 7 and 10 resembles LBBB (Left Bundle Branch Block) conduction — because there is a wide, monophasic R wave for the QRS of beat #1 in lead I — and there is predominant negativity for the QRS of beat #9 in leads V1, V2, V3. That said — the all-negative QRS for beat #4 in lead aVL is distinctly atypical for LBBB conduction.
- NOTE: Full review of aberrant conduction and the Ashman Phenomenon can be found at the bottom of the page in today's Addendum (which includes an Audio Pearl and Video Pearl on these topics).
 |
| Figure-4: The 12-lead ECG and long lead II rhythm strip in today's case. Has there been a recent infarction? (See text). |
- PEARL #5: In order to assess today's 12-lead ECG for signs of ischemia or infarction — we need to look in all 12 leads at those beats that are normally conducted with a narrow QRS complex. To do this — we need to focus on the appearance of beats #3, 6, 9 and 12 in other simultaneously-recorded leads (ie, We need to focus on those beats within the WHITE dotted-line rectangles in Figure-4).
- Unfortunately — beat #3 in the long lead II rhythm strip occurs at the same time that the standardization mark was recorded in leads I, II and III. As a result — we simply do not see what the QRST complex looks like in leads I and III.
- That said — the beat of most concern is beat #6. In lead aVL — beat #6 manifests a wide and deeply notched Q wave, ST segment coving with ever-so-slight ST elevation, and T wave inversion. In lead aVF — we see almost the mirror-image opposite picture, in the form of reciprocal ST depression with a terminal biphasic T wave. In association with the frequent PVCs (ie, ventricular trigeminy = every-third-beat is a PVC) — this raises concern for recent (if not acute) inferior MI.
- We get "4 looks" at the ST-T wave appearance in lead II (ie, beats #3, 6, 9 and 12 in the long lead II rhythm strip). Each of these beats supports our impression that there is reciprocal ST depression in the inferior leads.
- Assessment of QRST morphology in the anterior leads (leads V1, V2, V3) — shows small-but-present initial r waves in leads V2 and V3, and fairly unremarkable ST-T waves.
- QRST morphology in lateral chest leads V4, V5, V6 — is most suggestive of LV "strain", albeit R wave amplitude falls a bit shy of satisfying voltage criteria for LVH.
- CLICK on Figure-5 — which will magnify this Figure for you. Then advance one-by-one the next 5 Figures in the magnified mode to see our stepwise aproach for drawing this laddergram.
- For review on how to Read (and Draw) Laddergrams — See ECG Blog #188.
==============================
Acknowledgment: My appreciation to Hafiz Abdul Mannan Shahid (from Lahore, Pakistan) for the case and this tracing.
==================================
==============================
Relevant ECG Blogs to Today's Case:
- ECG Blog #185 — Use of a Systematic Approach to Rhythm Interpretation.
- ECG Blog #188 — How to Read (and Draw) Laddergrams.
- ECG Blog #70 — Reviews the Ashman Phenomenon (as a condition that predisposes to aberrant conduction).
- ECG Blog #71 — Reviews why the Ashman Phenomenon may be less reliable in AFib (ie, because of "concealed conduction").
- ECG Blog #211 — Reviews in detail WHY Aberrant Conduction occurs (and why RBBB aberration is the most common form).
- ECG Blog #140 — Example of alternating Bifascicular Block Aberration.
- ECG Blog #14 — Example of Blocked PACs.
- ECG Blog #15 — Example of a WCT due to Aberrant Conduction.
- ECG Blog #33 — Example of PACs with varying degrees of Aberrant Conduction.
============================
ADDENDUM (1/28/2022):
I've added below from previous Blog posts a series of educational material regarding the Ashman Phenomenon — and the basics of Aberrant Conduction.
Today’s ECG Media PEARL #29 (8:00 minutes Audio) — Reviews WHAT the Ashman Phenomenon is — HOW to use it clinically? — and — whether the Ashman phenomenon is accurate when the underlying rhythm is AFib?
- NOTE: For detailed review of the Ashman Phenomenon — with illustration of its clinical application — Please See ECG Blog #70. Use of the Ashman phenomenon with AFib is reviewed in ECG Blog #71.
=======================================
Today’s ECG Media PEARL #28 (4:45 minutes Video) — Reviews WHY some early beats and some SVT rhythms are conducted with Aberration (and why the most common form of aberrant conduction manifests RBBB morphology).
- NOTE #3: I have excerpted a 6-page written summary regarding Aberrant Conduction from my ACLS-2013-ePub. This appears below in Figures-11, -12, and -13).
- CLICK HERE — to download a PDF of this 6-page file on Aberrant Conduction.
 |
| Figure-11: Aberrant Conduction — Refractory periods/Coupling intervals (from my ACLS-2013-ePub). |
 |
| Figure-12: Aberrant Conduction (Continued) — QRS morphology/Rabbit Ears. |
 |
| Figure-13: Aberrant Conduction (Continued) — Example/Summary. |
==============================