This ECG is taken from chart audit of an older patient seen in the field. Unfortunately — many details of this case are lacking.
- How would YOU interpret this tracing?
- What diagnoses do you suspect?
 |
| Figure-1: ECG taken from chart audit of an older patient seen in the field (See text). |
=======================================
NOTE: Some readers may prefer at this point to listen to the 8:30-minute ECG Audio PEARL before reading My Thoughts regarding the ECG in Figure-1. Feel free at any time to refer to My Thoughts on this tracing (that appear below ECG MP-58).
=======================================
MY Sequential Thoughts on the ECG in Figure-1:
It's always challenging to try to interpret an ECG without benefit of the clinical history. Nevertheless — We are often asked to do so. Herewith follow my sequential thoughts on seeing this tracing, knowing only that this patient was found "in the field".
- The rhythm is obviously slow (ie, the rate is in the low 40s/minute). Although there is no long lead rhythm strip — the rhythm is surprisingly regular.
- Sinus P waves are seen in multiple leads, albeit these P waves are of very low amplitude (RED arrows in Figure-2).
- The PR interval is constant, albeit prolonged (ie, to at least 0.32 second) — therefore 1st-Degree AV Block.
- The QRS complex is very wide (ie, vertical BLUE lines in lead aVF suggest that the QRS complex is prolonged to ~0.20 second).
- QRS morphology is extremely unusual. It resembles LBBB in the limb leads (albeit with initial Q waves in leads I and aVL). In the chest leads — QRS morphology resembles RBBB (qR pattern in lead V1; wide terminal S wave in lead V6).
- There is marked left axis deviation (about -60 degrees) in the frontal plane.
- In addition to the Q waves in limb leads I and aVL — Q waves are also present in leads V1 and V2, with a tiny initial q wave in lead V3.
- There are marked ST-T wave abnormalities. These include ST elevation with T wave inversion in limb leads I and aVL — ST coving with T wave inversion in leads V2, V3 — and — an unusual coved-shape of ST elevation in lateral chest leads V4,V5,V6.
My Clinical Impression: The ECG findings in Figure-2 suggest 2 Diagnoses to me: i) Hyperkalemia until proven otherwise; and, ii) An associated acute evolving STEMI.
- Although the tall, peaked T waves with narrow base that are characteristic of hyperkalemia are not seen in today's ECG — other findings strongly suggest Hyperkalemia until proven otherwise. These include: a) Marked bradycardia; b) 1st-degree AV Block with a very prolonged PR interval; c) The tiny size of P waves; and, d) The marked QRS widening (ie, to 0.20 second) — with an unusual QRS morphology not resembling any known conduction disturbance.
- QRST Changes in 3 different lead areas suggest recent (if not actively ongoing) Infarction. High lateral leads I and aVL each show Q waves, ST elevation and T wave inversion (with subtle suggestion of reciprocal ST segment and T wave changes to lead aVL in lead III). Anterior leads V1,V2,V3 all show initial Q waves — with ST coving and T wave inversion in lead V2 — and ST coving with terminal T wave positivity in lead V3. Finally — each of the lateral chest leads (V4,5,6) show ≥2 mm of coved ST elevation.
 |
| Figure-2: I've labeled KEY findings from Figure-1 . The horizontal dotted RED lines in leads I, aVL; V4,V5,V6 show there is definite ST elevation with respect to the PR segment baseline (See text). |
CASE Follow-Up:
Chart audit revealed that this patient was unresponsive when found in the field. She died soon after emergency services (EMS) arrived. Because of her rapid demise — lab tests were not drawn. The terminal rhythm was PEA — with an extremely slow rhythm and a markedly widened QRS.
- I don't know if IV Calcium was given.
======================================
Important Points about HyperKalemia:
Rapid recognition of Hyperkalemia is among the most important of skills for emergency providers to master. The reasons for this are simple:
- i) Hyperkalemia is potentially life-threatening.
- ii) There is an empiric treatment (ie, IV Calcium) that can be life-saving — and which should often be given prior to lab confirmation of hyperkalemia, because cautious administration is safe — and not-to-promptly treat the patient risks losing the patient.
- iii) Not-to-recognize hyperkalemia as the cause of QRS widening, unusual rhythm disturbances and/or ST-T wave abnormalities will lead you down the path of potentially serious misdiagnosis.
PEARL #1: Be aware that IF you suspect potentially life-threatening hyperkalemia — that IV Calcium should be immediately given without the need to wait for lab confirmation.
- IV Calcium works fast (ie, within 2-3 minutes) by an action that stabilizes myocardial membrane potential, thereby reducing cardiac membrane excitability provoked by hyperkalemia (thereby protecting against cardiac arrhythmias). IV Calcium does not cause intracellular potassium shift, and it does not facilitate elimination of this cation.
- Either Calcium Chloride or Calcium Gluconate can be used (10 mL given IV over 3-5 minutes with ECG monitoring). NOTE: The chloride form contains 3X the amount of calcium per 10 mL dose (10 ml 10% CaCl = 6.8 mmol Ca++ vs 10 ml 10% CaGlu = 2.3 mmol Ca++).
- IV Calcium should be repeated IF there is no effect (ie, narrowing of the QRS on ECG) after 5-10 minutes. More of the gluconate form may need to be given (since it contains less calcium). The duration of IV Calcium is only ~30-60 minutes — but this should allow sufficient time for other treatments to be given.
- CaGlu can be given through a peripheral IV line. Because CaCl is more likely to cause tissue necrosis if there is extravasation — a central line is recommended (except if your patient is in cardiac arrest).
- Other treatments will often be needed (ie, Glucose/Insulin; Albuterol inhalation; Sodium Bicarbonate — and in refractory cases, hemodialysis) — but IV Calcium is the treatment of immediate choice for potentially life-threatening hyperkalemia.
- IV Calcium is not indicated for the treatment of peaked T waves with a narrow QRS and reasonable rhythm — as this is not a life-threatening situation.
The Textbook Sequence of ECG Changes:
For clarity — I've added Figure-3, which presents the "textbook" sequence of ECG findings seen with progressive degrees of hyperkalemia. While fully acknowledging that "not all patients read the textbook" — and that there will be variations in the various ECG findings from one patient-to-the-next — I have found awareness of the generalizations for these ECG signs in Figure-3 to be extremely helpful.
- The most common earliest sign of Hyperkalemia is T wave peaking. This may begin with no more than minimal K+ elevation (ie, K+ between 5.5-6.0 mEq/L) — although in some patients, T wave peaking won't be seen until much later (and in some patients — T wave peaking is never seen).
- PEARL #2: I love the image of the Eiffel Tower. With progressive degrees of hyperkalemia — the T wave (like the Eiffel Tower) becomes tall, peaked (pointed) with a narrow base. While patients with repolarization variants or acute ischemia (including the deWinter T wave pattern) often manifest peaked T waves — the T waves with ischemia or repolarization variants tend not to be as pointed as is seen with hyperkalemia — and, the base of those T waves tends not to be as narrow as occurs with hyperkalemia.
- PEARL #3: As helpful as I find Figure-3 is for providing insight to the ECG changes we look for when suspecting clinically significant hyperkalemia — progression from sinus rhythm to VFib as the 1st ECG sign of hyperkalemia has been documented. Not all patients read the textbook. (emDocs, 2017 — Management of Hyperkalemia).
 |
| Figure-3: The "textbook" sequence of ECG findings with hyperkalemia. |
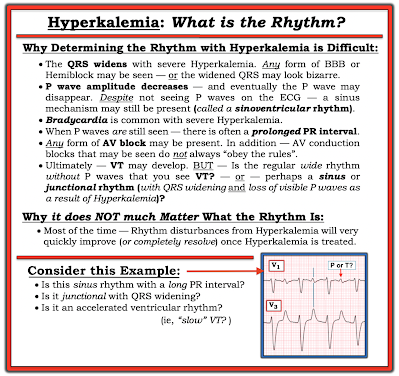
PEARL #4: Assessment of the rhythm with severe hyperkalemia is often extremely difficult because: i) As serum K+ goes up — P wave amplitude decreases, and eventually P waves disappear (See Panels D and E in Figure-3); ii) As serum K+ goes up — the QRS widens; and, iii) In addition to bradycardia — any form of AV block may develop (ie, AV conduction disturbances with severe hyperkalemia often do not "obey the rules" — See Figure-4).
- THINK for a MOMENT what the ECG will look like IF you can't clearly see P waves (or can't see P waves at all) — and the QRS is wide? ANSWER: The ECG will look like there is a ventricular escape rhythm, or like the rhythm is VT if the heart rate is faster.
- NOTE: P waves are extremely small in Figure-2. It is likely that with further increase in the serum K+ level — that P waves would no longer be seen. This would leave us with a slow rhythm without P waves, and with a very wide QRS complex — which would then be indistinguishable from a slow IVR (IdioVentricular Rhythm).
PEARL #5: As we have just noted, with progressive hyperkalemia — P wave amplitude decreases until ultimately P waves disappear. Interestingly, the sinus node is often still able to transmit the electrical impulse to the ventricles in such cases, even though no P wave may be seen on ECG. This is known as a sinoventricular rhythm.
PEARL #6: In my opinion, it is not worth wasting time trying to figure out the specific rhythm diagnosis of a bradycardia when there is hyperkalemia. I used to spend hours trying to do this — but after years of doing so, I finally realized: i) That a specific rhythm diagnosis is rarely possible when there is significant hyperkalemia — and, even if you succeed in making a diagnosis such as Wenckebach — chances are as serum K+ intra/extracellular fluxes change, that the cardiac rhythm will also soon change; and, ii) Clinically — it does not matter what the specific rhythm diagnosis is once you recognize hyperkalemia that needs to be immediately treated — because usually within minutes after giving IV calcium, the "bad" rhythm will probably "go away" (often with surprisingly rapid reestablishment of sinus rhythm).
 |
| Figure-4: Why assessing the rhythm with hyperkalemia is difficult (See text). |
PEARL #7: With marked hyperkalemia — it is impossible to know how much the elevated serum K+ is influencing QRS width and ST-T wave morphology until you normalize serum K+ and then REPEAT the ECG!
- For example — IF there was significant ST depression on the baseline tracing — then the "net effect" of such ST depression might sufficiently attentuate the T wave peaking of hyperkalemia in a way that produces "pseudo-normalization" of ST segments and T waves.
- Hyperkalemia may mask the ST-T wave changes of acute infarction. Alternatively — hyperkalemia may produce a "pseudo-STEMI" pattern that simulates acute infarction.
- With severe hyperkalemia — You can get an idea of the extent that excess serum K+ is altering the ECG by the improvement seen within minutes of giving IV Calcium. However, because the duration of action of IV Calcium is limited (ie, to ~30-60 minutes) — improvement of hyperkalemia-induced ECG changes following a dose of IV Calcium will be transient (until other measures produce a longer-lasting effect).
==================================
Final THOUGHTS regarding Today's CASE:
I was asked to interpret the ECG in Figure-1 in the "retrospectoscope" (ie, from the comfort of my desk armchair, sipping a cool drink as I viewed the tracing on my large screen desktop computer). This is admittedly a very different situation than being on-the-scene with an acutely ill patient under suboptimal conditions.
That said — the reason I immediately suspected severe hyperkalemia (despite the lack of T wave peaking)— was the combination of these 4 ECG findings:
- Marked bradycardia
- 1st-degree AV block with marked PR interval prolongation.
- The tiny size of P waves.
- Marked QRS widening (up to 0.20 second) — with an unusual QRS morphology not resembling any known form of conduction defect.
In addition — acute infarction was suggested by:
- Q waves, ST elevation and T wave inversion in leads I and aVL.
- Q waves in V1,V2 (tiny q in V3) — with ST-T wave changes in these leads that potentially were recent — plus — definite coved ST elevation in lateral chest leads.
My THOUGHTS in the Retrospectoscope:
- Given that this patient was unresponsive when found on the scene — one or more doses of IV Calcium was indicated (even before any labs might be drawn to confirm suspected hyperkalemia). There is little to lose by such treatment in this critical patient — and it might work if there was severe hyperkalemia.
- IF there was significant hyperkalemia — then improvement in the above ECG findings would be expected within minutes after giving IV Calcium — at which point decisions could be made on the likelihood of acute infarction.
- I have no idea if the above treatment might have helped in this case ...
==================================
Acknowledgment: My appreciation to David Didlake (USA) for allowing me to use this case and these tracings.
==================================
Related ECG Blog Posts to Today’s Case:
- ECG Blog #205 — Reviews my Systematic Approach to 12-lead ECG Interpretation.
- ECG Blog #185 — Reviews my Systematic Approach to Rhythm Interpretation (Assessment using the Ps,Qs & 3R Approach).
- ECG Blog #244 — Reviews a case of Hyperkalemia + Brugada Phenocopy.
- The January 26, 2020 post in Dr. Smith's ECG Blog — Reviews a number of examples of hyperkalemia (with My Comment at the bottom of the page).
- The September 5, 2020 post in Dr. Smith's ECG Blog — Reviews another case of Brugada Phenocopy from Hyperkalemia (with My Comment at the bottom of the page).
- The October 21, 2020 post in Dr. Smith's ECG Blog — Reviews a case of Hyperkalemia which highlights the difficulty of determining the Rhythm (with My Comment at the bottom of the page).
- NOTE: There are links to numerous cases of life-threatening Hyperkalemia with "other" ECG findings (beyond tall peaked T waves) — in the excellent January 16, 2022 post by Drs. Meyers & Smith, in Dr. Smith's ECG Blog. Please also check out MY COMMENT at the very bottom of this page!


No comments:
Post a Comment