- HOW would YOU interpret the ECG in Figure-1 — if no clinical information was provided?
-USE.png) |
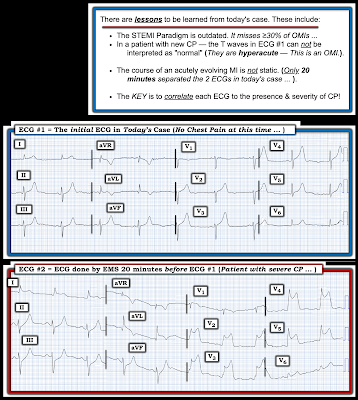
| Figure-1: The initial ECG in today's case. (To improve visualization — I've digitized the original ECG using PMcardio). |
- The "good news" — is that after an extended hospitalization, the patient was finally discharged home, and doing well.
- At 1st glance of the chest leads — the QRS complex appears to be significantly widened. However, on looking closer at leads V1 and V6 — and especially at the QRS in the limb leads — it becomes apparent that the QRS is probably of normal duration!
- But — IF the QRS is not prolonged — this means that we are looking at perhaps the greatest amount of ST segment elevation in lead V3 that I (and perhaps you) have ever seen! (that attains more than 40 mm in lead V4).
- As discussed in ECG Blog #364 and ECG Blog #265 — We are looking at "Shark Fin" ST elevation!
- "Shark Fin" ST segment elevation is most often a sign of severe transmural ischemia that results from acute coronary occlusion. Today's case is different in that profound myocardial injury (from electrocution) rather than acute coronary occlusion is the cause of this ECG pattern.
- PEARL: The KEY for confirming that "Shark Fin" morphology is the cause of the striking ECG picture in Figure-1 — is to find 1 or 2 leads in which you can clearly define the limits (end point) of the QRS complex. The most helpful leads for clarifying the end point of the QRS in today's case are lead V1 and lead V6.
- Note in Figure-2 — that I've drawn in a RED line parallel to the heavy ECG grid line in the simultaneously-recorded chest leads. By choosing the end point of the QRS that is clearly visible in leads V1 and V6 — I'm able to define the end point of the QRS complex in the other chest leads ( = leads V2-thru-V5), knowing that the ST segment begins just to the right of this vertical RED line.
- Alternatively — the shape of the ST elevation in lead V2 might also be consistent with a component of Brugada Phenocopy (See ECG Blog #238). That said, even if true — ST elevation in the remaining chest leads is still virtually certain to represent "shark fin" ST elevation from severe myocardial injury.
==========================================
Acknowledgment: My appreciation to Hamdallah Naser (from AL-Najaf, Iraq) for the case and this tracing.
==========================================
![]()
=====================================
- The Audio Pearl below reviews the concept of "shark fin" ST elevation.
ECG Media PEARL #73 (5:40 minutes Audio) — Reviews the concept of "Shark Fin" ST elevation and depression as a sign of extensive acute infarction.
==============================
Additional Relevant ECG Blog Posts to Today’s Case:
- ECG Blog #185 — Reviews my System for Rhythm Interpretation, using the Ps, Qs & 3R Approach.
- ECG Blog #265 and ECG Blog #364 — Review cases of Shark-Fin ST Elevation.

-USE.png)

-USE.png)
-USE.png)
-USE.png)
-USE.png)




-USE.png)

-USE.png)







-USE.png)
-USE.png)
-USE.png)
-USE.png)





-USE.png)





