The ECG shown in Figure-1 was obtained from an older patient with known coronary disease, who presented with a 10-hour history of worsening chest pain.
- Given the above history — How would YOU interpret this tracing?
- Should the cath lab be activated?
- Extra Credit: Can you envision a clinical "story" to explain all ECG findings?
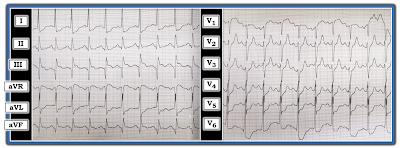 |
| Figure-1: ECG obtained from an older patient with known coronary disease and chest pain of ~10 hours duration (See text). |
=======================================
NOTE: Some readers may prefer at this point to listen to the 10:20-minute ECG Audio PEARL before reading My Thoughts regarding the ECG in Figure-1. Feel free at any time to refer to My Thoughts on this tracing (that appear below ECG MP-70).
=======================================
Today’s ECG Media PEARL #70 (10:20 minutes Audio) — Reviews HOW to "Date" an Infarction based on the initial ECG.
MY Sequential Thoughts on the ECG in Figure-1:
As always — I favor the use of a Systematic Approach (which I review in ECG Blog #205). Use of a systematic approach is especially important in today's case — because there are multiple ST-T wave abnormalities that otherwise might be easy to overlook.
- Rate & Rhythm: The heart rate is fast. The P wave is upright in lead II, with a fixed and normal PR interval — so the rhythm in Figure-1 is sinus tachycardia at ~120-125/minute.
- Intervals (PR/QRS/QTc): The PR interval is normal — the QRS complex is narrow — and, the QTc may be slightly prolonged (albeit difficult to assess the QTc interval when the heart rate is faster than 90-100/minute).
- Axis: The frontal plane QRS axis is normal (I'd estimate at about +20 degrees — given slightly more net positivity in lead I compared to lead II, with a near-isoelectric QRS in lead III).
- Chamber Enlargement: The standardization marker is missing — so the best we can do is to assume normal standardization. Regardless of the standardization — I suspect there is LVH (Left Ventricular Hypertrophy) — given the tall R wave in lead I (which is cut off — but looks to be at least 15 mm) — and especially given the very tall R wave in lead V6 (of at least 20 mm — though as shown in Figure-2, precise measurement is difficult given overlap with the QRS in leads V4 and V5) — See ECG Blog #245 for details on LVH criteria.
Regarding Q-R-S-T Changes:
- Q Waves — There are very large Q waves in 2 of the 3 inferior leads (ie, in leads III and aVF) — with a smaller-but-definitely-present Q wave in the 3rd inferior lead ( = lead II). T
- R Wave Progression — Transition (where the R wave becomes taller than the S wave is deep) is appropriate, occurring between leads V3-to-V4. There may be a slight chest lead placement error for lead V2 (since the R wave and S wave in this lead are both larger than the R and S waves in both neighboring leads = V1 and V3, and normally that should not be). That said — even if present, this slight lead placement error should not alter the overall interpretation of this tracing.
- ST-T Wave Changes — There is significant ST elevation of coved shape in lead III. There is abnormal ST elevation of a lesser degree (with a similar shape) in lead aVF. However, there is no ST elevation in the 3rd inferior lead (which is lead II). There is 1-2 mm of ST elevation in lead aVR.
- T waves are surprisingly tall and peaked in leads V2 and V3, and to a lesser extent in lead V4. Unlike what occurs with hyperkalemia — there is no T wave peaking in any of the other 9 leads on this tracing.
- There is marked ST depression in 5 of the remaining leads (ie, in leads I, aVL; V4, V5,V6).
Putting It All Together: There is a lot going on in this case. Although I lack details of follow-up for this patient — I nevertheless thought it worthwhile to work through what I feel is the most logical clinical scenario — as I believe the brief History we are given and this single ECG do tell a Story. BOTTOM LINE — I thought the ECG in Figure-1 strongly suggests there has been a recent (if not still acutely ongoing) infero-postero STEMI ( = ST Elevation Myocardial Infarction). I'll add the following thoughts:
- The History we are given (namely that the patient is an older adult with known coronary disease — who presented with a 10-hour history of worsening chest pain) — is essential for optimal assessment and clinical decision-making.
- Given this history and this patient’s ECG — there should be no doubt that inferior MI has occurred at some point in time. Large Q waves are seen in each of the 3 inferior leads (especially in leads III and aVF). That said — the clinical challenge is to determine, "What happened when?" — and — whether the cath lab should be immediately activated?
- Of clear concern is the surprisingly fast rate of this patient's sinus tachycardia (ie, between 120-125/minute). Uncomplicated infarction would not be expected to cause a tachycardia this fast — which raises the concern that this patient may be decompensating (ie, pehaps in severe heart failure? — and/or with some other issue requiring immediate attention).
So HOW can we “date” this patient’s inferior MI? "Dating" an infarction is challenging! I address this question in the above Audio Pearl #70. There is conflicting evidence on this tracing with regard to the "age" of infarction.
- The extremely large Q waves in leads III and aVF favor prior infarction. That said — it is possible that this older patient with known coronary disease had a previous inferior infarction — and is now having acute reinfarction of the inferior wall. PEARL: On occasion, significant Q waves have been known to form in as little as 1-to-2 hours. THEREFORE: We can not rule out the possibility of a very recent, or even acute ongoing infarction simply on the basis of the large size of these inferior Q waves.
- There is coved ST elevation in lead III — and to a lesser extent in lead aVF. In addition — there is marked ST depression in no less than 5 leads (ie, leads I, aVL; V4, V5 and V6). This ST depression is clearly more marked and of a different "shape" than would be expected simply from LVH with "strain". I therefore interpreted this as reciprocal and/or ischemic ST depression from an acute (potentially ongoing) coronary event until proven otherwise.
- In further support of a recent (if not acute) cardiac event — is the "magical" mirror-image opposite relationship of ST-T waves in leads III and aVL. As discussed in ECG Blog #184 and illustrated by the "mirror test" inserts I added for leads III and aVL in Figure-2 — the mirror-image of the ST-T wave depression in lead aVL looks identical to the ST elevation seen in lead III. Similarly — the mirror-image of the ST-T wave elevation in lead III looks identical to the shape of the ST depression seen in lead aVL.
- That said — against the inferior infarction being acute is the fact that the amount of ST elevation in lead aVF is no more than minimal — and the complete lack of any ST elevation in lead II. Given the amount of ST depression in multiple leads on this tracing — I would have expected definite ST elevation of comparable amount in the inferior leads IF the infarction was acute.
- A striking finding is the T wave peaking seen in leads V2 and V3. We see a continuation of this unexpectedly marked T wave peaking (following depression of the ST segment) in lead V4. This is not the T wave peaking of hyperkalemia — since it is only present in these 3 leads (and we’d expect more generalized T wave peaking if there was hyperkalemia). Instead — I feel the most logical explanation is illustrated by the "mirror test" inserts added in Figure-2 for leads V2 and V3 — which suggest that the mirror-image of the peaked T waves in leads V2, V3, V4 most likely represents deeply inverted reperfuson T waves from recent posterior infarction (this concept further reviewed in ECG Blog #193).
- Finally — we are left with ST elevation in lead aVR — which, in association with the marked ST depression in 5 of the remaining leads (ie, leads I, aVL; V4,5,6) — raises concern for diffuse subendocardial ischemia resulting from significant coronary disease in other anatomic areas.
My SYNTHESIS (Explaining All ECG Findings in Today's Case):
The ECG findings in today's case can not be explained by a single acute event. Instead — I suspect the following:
- This patient had a recent, large infero-postero STEMI. The limited amount of ST elevation in inferior leads — in association with surprisingly tall, peaked anterior T waves suggest there has been some spontaneous reperfusion (and that infarction occurred at least a number of hours ago — which is supported by the history stating that chest pain has been present for 10 hours).
- This patient most probably has multi-vessel disease — with the marked ST depression in multiple leads potentially representing ischemia in other anatomic areas (and potentially attenuating ST elevation that otherwise may have been seen).
- There is LVH — but the shape and amount of ST depression in lateral leads represents more than just LV "strain".
- The marked sinus tachycardia (of ~120-125/minute) — in association with the above ECG findings and persistence of chest pain (worsening over 10 hours) — are clear indication for activating the cath lab! Even though there is ECG evidence for reperfusion — what has recently reopened might once again close — and — the marked sinus tachycardia + marked ST depression in multiple leads + persistent and worsening chest pain all argue for promptly defining the anatomy to determine IF there is need for acute PCI (Percutaneous Coronary Intervention).
==============================
ADDENDUM (10/28/2021) — There are elements of this case that closely resemble Aslanger's Pattern (This pattern is very nicely described by Dr. Smith in his January 4, 2021 post). The premise of Aslanger's — is that IF there is inferior MI + diffuse subendocardial ischemia — then the vector of ST elevation will shift rightward. This results in:
- ST elevation in lead III (as a result of the acute inferior MI) — but not in the other inferior leads (II, aVF) because of the rightward shift in the ST elevation vector.
- ST depression in one or more of the lateral chest leads (V4, V5, V6) with a positive or terminally positive T wave — but without ST depression in lead V2. (Marked ST depression from multi-vessel coronary disease serves to attentuate what would have been ST elevation in leads II and aVF).
- ST elevation in lead V1 that is more than any ST elevation in lead V2.
- There may be more reciprocal ST depression in lead I than in lead aVL (because of the rightward ST vector shift).
- The only leads showing significant ST elevation may be leads III, aVR and V1 (reflecting the inferior MI + subendocardial ischemia from diffuse coronary disease).
The above said — additional features to consider in today's case include: i) There is also marked LVH; and, ii) The infero-postero MI is probably at least 10 hours old, and is now showing prominent reperfusion T waves in the posterior distribution (ie, tall, peaked anterior T waves).
==============================
Acknowledgment: My appreciation to Ahmad Separham (from Tabriz, Iran) for the case and this tracing.
==================================
Related ECG Blog Posts to Today’s Case:
- ECG Blog #205 — Reviews my Systematic Approach to 12-lead ECG Interpretation.
- ECG Blog #245 — Reviews "My Take" on a user-friendly approach to the ECG diagnosis of LVH (including CAVEATS that may complicate assessment of associated acute ischemia).
- ECG Blog #142 — Presents another case for discussion on how to "date" an infarction.
- ECG Blog #193 — illustrates use of the Mirror Test to facilitate recognition of acute Posterior MI. This blog post reviews the basics for predicting the "culprit artery". NOTE: Figure-5 in the Addendum of this blog post illustrates the essentials for identifying an isolated posterior MI.
- ECG Blog #184 — illustrates the "magical" mirror-image opposite relationship with acute ischemia between lead III and lead aVL (featured in Audio Pearl #2 in this blog post).
- The September 21, 2020 post in Dr. Smith's ECG Blog — My Comment (at the bottom of the page) emphasizes utility of the Mirror Test for diagnosis of acute Posterior MI.
- The February 16, 2019 post in Dr. Smith's ECG Blog — My Comment (at the bottom of the page) emphasizes utility of the Mirror Test for diagnosis of acute Posterior MI.
- ECG Blog #80 — reviews prediction of the "culprit" artery (and provides another case illustrating the Mirror Test for diagnosis of acute Posterior MI).



No comments:
Post a Comment