The ECG in Figure-1 was obtained from a man in his mid-30s, who presented to the ED with new-onset chest pain that began 1 hour earlier.
- How would you interpret this tracing?
- What is the “culprit” artery?
 |
| Figure-1: Initial ECG in the ED from a man in his mid-30s with new-onset chest pain (See text). |
=======================================
NOTE: Some readers may prefer at this point to listen to my 12-minute ECG Audio PEARL before reading My Thoughts regarding the ECG in Figure-1. Feel free at any time to review My Thoughts on ECG #1 (that appear below ECG MP-10).
=======================================
MY Thoughts on ECG #1:
Obviously — ECG #1 shows an acute STEMI. I thought the interesting part of today’s case was reflection on the 2nd Question that I posed — namely, predicting the “culprit” artery.
- The rhythm in ECG #1 looks to be a fairly regular sinus rhythm at ~85/minute. All intervals (PR, QRS, QTc) are normal.
- Did YOU notice the RAD (Right Axis Deviation)? Although tiny in size — the QRS complex in lead I is predominantly negative — and a qR pattern is seen in each of the inferior leads. This morphology is consistent with LPHB (Left Posterior HemiBlock) — which is relevant as a new-onset conduction defect in this patient with a large acute STEMI.
- There is no chamber enlargement.
Regarding Q-R-S-T Changes:
- A small Q wave with significant ST elevation is seen in each of the 3 inferior leads (ie, leads II, III, aVF). The T waves in leads II and aVF are hyperacute (ie, clearly “fatter”-at-their peak than expected).
- Although difficult to tell if there is (or is not) ST elevation in lead I — the T wave in this lead is remarkable for being huge (!) with respect to the tiny QRS complex, and clearly hyperacute (much fatter-at-its-peak and wider-at-its-base than expected, given how tiny QRS amplitude is in this lead).
- Remarkable for its absence — is the lack of significant ST-T wave change in lead aVL.
- There is ST depression in leads V1 and V2, with an unexpectedly tall T wave in lead V2. Subtle-but-relevant are the taller-than-expected initial R waves in leads V2 and V3 (R wave amplitude in lead V1 almost equals S wave depth in this lead — and that is not a “normal” finding). In the setting of acute inferior STEMI — the ST-T wave findings in leads V1 and V2 are consistent with a positive “Mirror Test” — and are diagnostic of acute posterior MI (See Figure-2).
- There is beginning ST elevation in lead V4 — which becomes marked ST elevation in leads V5 and V6.
- NOTE: Small and narrow Q waves are seen in leads V5 and V6. Although the finding of small and narrow “septal” q waves is common and normal in asymptomatic individuals — in association with the dramatic acute changes in ECG #1, these lateral chest lead Q waves may indeed be a harbinger of more injury to come.
Putting It All Together:
The ECG in Figure-1 is consistent with an acute infero-postero-lateral STEMI.
- Small q waves are forming in infero-lateral leads — and LPHB appears to be present.
- This picture is highly suggestive of acute occlusion of a dominant LCx (Left Circumflex) Artery because: i) ST elevation is significantly more in lead II compared to lead III (whereas with acute RCA occlusion — ST elevation is typically more in lead III>II); ii) There is essentially no reciprocal ST depression in lead aVL (whereas with acute RCA occlusion — there is almost always significant reciprocal ST depression in lead aVL); and, iii) There is marked ST elevation in lateral chest leads V5 and V6, with ST elevation beginning as early as lead V4 (whereas with RCA occlusion — the relative amount of any lateral chest lead ST elevation seen is almost always less than the amount of ST elevation in lead III).
Follow-Up to this Case:
The facility where this patient was seen did not have acute cardiac catheterization capability. The patient was instead immediately treated with thrombolytic therapy — and had an excellent clinical result from this.
- NOTE: I use the follow-up ECG to this case (obtained within an hour of starting thrombolytic therapy) as the "theme" for my next post in ECG Blog #194 — It is a very challenging and insightful arrhythmia!
=======================================
Acknowledgment: My appreciation to Hosain Saleh (from Damascus, Syria) for the case and this tracing.
=======================================
ADDENDUM:
- I thought today’s case to be an excellent lead-in for putting together a series of links, images and PDFs relevant to the coronary anatomy — detection of the “culprit” artery — assessment of some other acute coronary syndromes — and for making the case for replacing the term “STEMI” with “OMI” in the hope of substantially increasing detection of acute coronary occlusion.
Free PDF Downloads from relevant Sections in my ECG-2014-ePub:
- PDF File: Overview on the Cardiac Circulation and the “Culprit” Artery in Acute MI —
- PDF File: Posterior MI and the “Mirror Test” —
- PDF File: Takotsubo Cardiomyopathy —
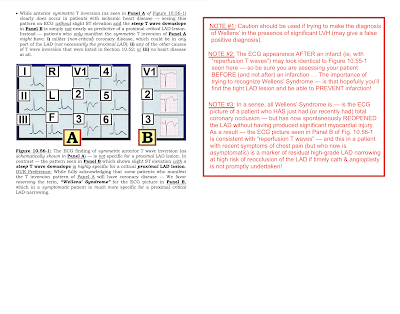
 |
| Figure-3: ECG findings to look for when your patient with new-onset cardiac symptoms does not manifest STEMI-criteria ST elevation on ECG. For more on this subject — SEE the September 3, 2020 post in Dr. Smith’s ECG Blog with 20-minute video talk by Dr. Meyers on The OMI Manifesto. For my clarifying Figure illustrating T-QRS-D (2nd bullet) — See My Comment at the bottom of the page in Dr. Smith’s November 14, 2019 post. |
===================================
Relevant ECG Blog Posts
- ECG Blog #184 — That magical inverse relationship between leads III and aVL.
- ECG Blog #167 — More on that "magical" lead III-aVL relationship.
- ECG Blog #183 — deWinter-like T waves
- ECG Blog #190 — Acute RV MI
- ECG Blog #56 — Posterior MI; Mirror Test
- ECG Blog #80 — What’s the Culprit Artery? + the Mirror Test
- ECG Blog #82 — What’s the Culprit Artery?
- ECG Blog #162 — What’s the Culprit Artery?
- ECG Guru (9/3/2019) — See My Comment regarding acute occlusion of 1st or 2nd Diagonal Branch of the LAD.
- The importance of the new OMI (vs the old STEMI) Paradigm — See My Comment in the July 31, 2020 post in Dr. Smith's ECG Blog.
- Acute OMI that wasn’t accepted by the Attending — See My Comment at the bottom of the page in the November 21, 2020 post on Dr. Smith’s ECG Blog.
- Another overlooked OMI (Cardiologist limited by STEMI Definition) — See My Comment at the bottom of the page in the September 21, 2020 post on Dr. Smith’s ECG Blog.
- Recognizing hyperacute T waves — patterns of leads — an OMI (though not a STEMI) — See My Comment at the bottom of the page in the November 8, 2020 post on Dr. Smith's ECG Blog.
- Recognizing T-QRS-D (Terminal QRS Distortion) as a sign of acute OMI — See My Comment at the bottom of the page in the November 14, 2019 post on Dr. Smith's ECG Blog.
- LVH vs a Repolarization variant vs LAD OMI (and looks like Wellens' after reperfusion) — See My Comment at the bottom of the page in the October 23, 2020 post on Dr. Smith's ECG Blog.
- Repolarization Variant vs Acute OMI (even repolarization variants may sometimes manifest "dynamic" ECG changes!) — See My Comment in the August 22, 2020 post on Dr. Smith's ECG Blog.
- Diagnosis of an OMI from the initial ECG — Serial tracings with spontaneous reperfusion — then reocclusion! — See My Comment at the bottom of the page in the October 14, 2020 post on Dr. Smith's ECG Blog.
- And for more on the Mirror Test — See My Comment at the bottom of the page in the September 21, 2020 post and, in the February 16, 2019 post on Dr. Smith's ECG Blog.
===================================
 |
| Figure-4: Regarding the variable ECG findings with LMain Occlusion. (NOTE: These findings are summarized from the August 9, 2019 post in Dr. Smith's ECG Blog). |
 |
| Figure-5: Isolated posterior MI. |
 |
| Figure-6: Summary of Wellens’ Syndrome (Pages 1-2). |
 |
| Figure-7: Summary of Wellens’ Syndrome (Pages 3-4). |




It's really an interesting case to learn from.
ReplyDeleteThank you very much!
THANK YOU Hosain for contributing this case! — :)
DeleteGreat
ReplyDelete:)
Delete