The ECG shown in Figure-1 was obtained from a young adult who presented with a presyncopal episode.
- What is the cause of the AV dissociation?
 |
| Figure-1: ECG from a young adult who presented with a presyncopal episode. |
My Initial Thoughts on Seeing this Tracing:
When I first saw this ECG — my "eye" was immediately drawn to the deflections that I highlight with BLUE arrows in Figure-1. I initially thought this tracing had to represent some unusual form of AV dissociation.
- CONFESSION: This is a trick tracing! I fully acknowledge that I deliberately chose this tracing to illustrate how easy it is to be fooled by artifact. My goal for this post is to review some of the ways to rapidly recognize when artifact is present — since this is usually not taught "in the textbook".
=======================================
NOTE: Some readers may prefer at this point to listen to the 7:45-minute ECG Audio PEARL before reading My Thoughts regarding the ECG in Figure-1. Feel free at any time to refer to My Thoughts on this tracing (that appear below ECG MP-18).
=======================================
Today’s ECG Media PEARL #18 (7:45 minutes Audio) — Reviews recognition of Artifact — and — using Einthoven's Triangle to determine within seconds the "culprit" extremity causing the Artifact on your ECG (This Audio Pearl was first published in ECG Blog #201. That blog post illustrates a case in which artifact is initially mistaken for acute ST elevation).
HOW Did I Know there was Artifact in Figure-1?
There are several clues that strongly suggest the BLUE arrow deflections in Figure-1 are not P waves at all — but instead, are pointing to artifact. These clues include:
- The shape of these deflections is geometric. That is — these deflections in each of the inferior leads are much taller than is usually seen for P wave amplitude. These deflections consist of a very steep and straight upward line that ends in a point. It is distinctly unusual to see a physiologic P wave with such a sharp point despite having such a narrow base. Elsewhere, in leads aVR and aVL — these deflections appear as a short, negative skinny line. Physiologic P waves virtually always have at least some width (and should not appear as a very thin, vertical line). This "geometric" appearance of these deflections looks like artifact (and when unusual-looking deflections "look like" artifact — this is because they usually are artifact).
- As suggested by the BLUE arrows in the long lead II rhythm strip — the distribution of these deflections does not make physiologic sense. It is possible for atrial and junctional rhythms to be dissociated with nearly equal rates. This occurs with isorhythmic AV dissociation (See ECG Blog #195), in which P waves and junctional QRS complexes may move with respect to each other's position, but still appear close to each other throughout the duration of the rhythm strip. In contrast, in Figure-1 — the BLUE-arrow deflections appear in all phases of the R-R interval. And while it is possible for there to be complete AV block — this usually does not occur with both atrial and junctional rates being as fast as they are in Figure-1.
- Underlying sinus P waves are regularly seen in several of the leads in Figure-1. The BEST clue for recognizing artifact — is being able to identify the underlying original rhythm that continues unaffected by the deflections you suspect are artifact. These regularly-occurring normal P waves are best seen in lead I of Figure-1.
- The relative size of the deflections in Figure-1 that are suspected of being artifact manifest the precise relative dimensions expected when artifact is caused by a "culprit" extremity (as shown within the colored circles in Figure-2).
PEARL #1: The relative size and distribution of artifact deflections in Figure-2 precisely follow the location and relative amount of amplitude distortion predicted by Einthoven’s Triangle. By this I mean:
- The height of the artifact spike is approximately equal in 2 of the limb leads (ie, in leads II and III) — and, not seen at all in the 3rd limb lead (ie, no artifact at all is seen in lead I). By Einthoven’s Triangle (See the above picture posted with today’s ECG Media Pearl — which shows Einthoven’s Triangle in the righthand corner) — the finding of equal artifact amplitude in Lead II and Lead III, localizes the “culprit” extremity to the LL ( = Left Leg) electrode.
- The absence of any artifact at all in lead I is consistent with this — because, derivation of the standard bipolar limb lead I is determined by the electrical difference between the RA ( = Right Arm) and LA ( = Left Arm) electrodes, which will not be affected if the source of the artifact is the left leg.
- As I discuss in detail in my MP-18 Audio Pearl above — the finding of maximal amplitude artifact in unipolar lead aVF confirms that the Left Leg is the “culprit” extremity.
NOTE: I reproduce below in Figures 5, 6 and 7 — the 3-page article by Rowlands and Moore (J. Electrocardiology 40: 475-477, 2007) — which is the BEST review I’ve seen on the physiology explaining the relative size of artifact amplitude deflections when the cause of the artifact is arising from a single extremity. These principles are illustrated in Figure-2:
- As noted by the equations on page 477 in the Rowlands and Moore article: i) The amplitude of the artifact is maximal in the unipolar augmented electrode of the “culprit” extremity — which is lead aVF in Figure-2 (contained within the BLUE circle); and, ii) The amplitude of the artifact in the other 2 augmented leads (ie, leads aVR and aVL) is about 1/2 the amplitude of the artifact in lead aVF (contained within the RED circles in Figure-2).
- Similarly — the amplitude of the artifact deflections in the 6 unipolar chest leads in Figure-2 is also significantly reduced from the maximal amplitude seen in leads II, III and aVF (contained within the YELLOW circles in Figure-2).
PEARL #2: As alluded to earlier, the BEST clue for confirming that suspicious deflections are truly the result of artifact — is IF you are able to identify the underlying original rhythm that continues unaffected by the deflections you suspect are artifact.
- RED arrows in Figure-3 clearly show continuation of the underlying regular sinus rhythm. This is easiest to see in lead I — because no artifact is seen in this lead. From the 3 sinus P waves in lead I — it can be seen that a regular P-P interval continues for the 4 on-time sinus P waves that are then seen after the lead change in lead aVR (RED arrows in lead aVR).
- Vertical PURPLE lines in the long lead II rhythm strip highlight regularly-occurring sinus P waves that are unrelated to the BLUE-arrow artifact deflections. This proves these deflections represent artifact.
PEARL #3: The goals of identifying the source and cause of artifact are: i) To avoid erroneous interpretation of the ECG (For example, there is no AV dissociation in today's case!); and, ii) To hopefully fix the cause of the artifact so that a better quality tracing can be obtained.
- The above deductive process identifies the source of the artifact in today's tracing as coming from the Left Leg.
- The fact that the artifact in today's case is completely unrelated to the QRS complex (ie, BLUE arrows in Figure-3 occur at all points in the cardiac cycle) — rules out causes related to cardiac contraction (such as contact of a lead electrode with a pulsating artery).
- Clinically — Now that we know that the artifact arises from something occurring in the patient's left leg — the BEST way to determine the cause of this artifact would be to GO to the bedside and LOOK at the patient (with special attention paid to the patient's left leg, in the hope of identifying the cause of the repetitive artifact activity).
FOLLOW-UP to Today's Case: For clarity — I've added a 2nd ECG done the same day on today's patient (Figure-4).
- Similar small-amplitude sinus P waves with the same slightly shortened PR interval are seen in ECG #2, as were seen in the initial ECG #1. But note that there is no longer any artifact seen in ECG #2 (ie, in the bottom tracing in Figure-4).
- The fact that P wave morphology in ECG #2 is identical to those sinus P waves that we were able to see in ECG #1 (RED arrows in the initial ECG) — provides additional confirmation that the geometric-looking deflections (highlighted by BLUE arrows in ECG #1) were in fact the result of some kind of artifact arising from the patient's left foot.
- P.S. — You may have noticed (and been impressed by) the marked increase in QRS amplitude and anterior lead ST-T wave changes seen in both ECG #1 and ECG #2. These tracing were obtained from the same patient I presented in my previous ECG Blog #254. As discussed in the conclusion to that case — these ECG findings did not represent Wellens' Syndrome, nor HCM (Hypertrophic CardioMyopathy), nor LVH — but instead, by exclusion — were felt to represent a repolarization variant.
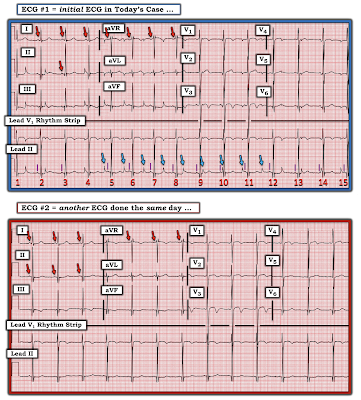 |
| Figure-4: I've added a 2nd ECG done the same day on this patient (See text). |
BOTTOM LINE: You will see artifact frequently in your real-life clinical work. With a little practice, you can get good at rapidly recognizing that unusual deflections (such as those seen in today's case) — are the result of some form of artifact.
- Nothing else shows the mathematical relationships described above, in which there is equal maximal artifact deflection in 2 of the 3 limb leads (with no artifact at all in the 3rd limb lead) — in which maximal artifact in the unipolar augmented lead will be seen in the extremity electrode that shares the 2 limb leads with maximal artifact (according to Einthoven’s Triangle).
- Determining if artifact deflections manifest a fixed relationship to the QRS complex (as was seen in ECG Blog #201) — vs being totally unrelated to neighboring QRS complexes (as was the case in today's tracing) — will instantly tell you IF artifact deflections are related to cardiac contraction (or arterial pulsations) — or — IF artifact is related to some local causative factor.
 |
| Figure-5: Page 475 from the Rowlands and Moore article referenced above (See text). |
 |
| Figure-6: Page 476 from the Rowlands and Moore article referenced above (See text). |
 |
| Figure-7: Page 477 from the Rowlands and Moore article referenced above (See text). |
==============================
Acknowledgment: My appreciation to Ghady Rahhal (from Virginia, USA) for the case and this tracing.
==================================
==============================
Additional Relevant ECG Blog Posts to Today’s Case:
- ECG Blog #201 — Reviews a case of Artifact due to arterial pulsations (with derivation of the "culprit" extremity).
- ECG Blog #195 — Reviews the phenomenon known as isorhythmic AV Dissociation (in which the atrial and junctional [or ventricular] rate is virtually equal, but P waves are not conducting to the ventricles).
Regarding ECG Recognition of ARTIFACT:
- ECG Blog #148 — Artifact simulating VFib.
- ECG Blog #44 — Artifact produced by Parkinsonian tremor
- ECG Blog #139 — Artifact simulating AFlutter.
- ECG Blog #132 — More artifact simulating VT-VFib.
- Brief review by Tom Bouthillet on some common causes of artifact.
Finally — I link to several illustrative Cases taken from Dr. Smith’s ECG Blog. For each of these posts — Please scroll down to the bottom of the page to see My Comment. These cases provide insight to assessment for ARTIFACT:
- The September 27, 2019 post in Dr. Smith’s ECG Blog — for an example of how to recognize the source of extremity artifact.
- The October 17, 2020 post in Dr. Smith’s ECG Blog — for an example of VT-like artifact
- The January 30, 2018 post in Dr. Smith’s ECG Blog — for arterial pulsation artifact (Please click on the COMMENTS to this post to see my discussion).





No comments:
Post a Comment