The ECG in Figure-1 was obtained from a 60-ish man who was seen in the field by EMS for new-onset chest pain. No prior cardiac history.
- Should you activate the cath lab?
- IF so — What would expect to find on cath?
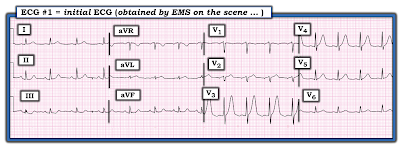 |
| Figure-1: The initial ECG obtained by EMS on the scene. |
My THOUGHTS on ECG #1:
As always — I interpreted ECG #1 by use of a Systematic Approach (See ECG Blog #205 for details):
- Rate & Rhythm: There is a regular sinus rhythm (with upright conducting P waves in lead II) — at a rate of ~100/minute (therefore sinus tachycardia).
- Intervals (PR, QRS, QTc) — The PR interval is normal, and the QRS complex is not widened. Given the fairly fast heart rate — I suspect tht the QTc is not prolonged.
- Axis: Normal (about +50 degrees).
- Chamber Enlargement: None.
Regarding Q-R-S-T Changes:
- Q Waves: There appear to be very small q waves in inferior and lateral chest leads. These are unlikely to be of clinical significance.
- R Wave Progression: Transition (where height of the R wave exceeds depth of the S wave in the chest leads) occurs normally (ie, between leads V2-to-V3). There may be malposition of lead V2 — because the r wave in lead V2 looks smaller than the r wave in lead V1, before becoming unusually tall with the abrupt transition that occurs in lead V3. In addition — the P wave in leads V1,V2 is negative (before becoming decidedly positive in lead V3) — and — QRS morphology looks similar in leads aVR, V1 and V2 (I discuss CLUES for recognition of too-high placement of the lead V1 and V2 electrodes in My Comments at the BOTTOM of the page in the November 4, 2018 and March 29, 2020 posts in Dr. Smith's ECG Blog).
Regarding ST-T Wave Changes:
- By far — The most remarkable finding on this tracing is the overly prominent T waves in leads V3 and V4. The T wave in lead V3 is pointed in shape and huge in size! (It measures no less than 12-13 mm — and is taller than the fairly tall R wave in this lead).
- Although the T wave in lead V4 is no longer taller than the corresponding R wave in this lead — it still looks taller-than-it-should-be, in addition to being peaked in shape with a wider-than-expected base. Thus, in a patient with new-onset chest pain — the T waves in leads V3 and V4 should be seen as "hyperacute" until proven otherwise (See Audio Pearl-35a below).
- PEARL #1: Viewed by itself — the T wave in lead V5 might not necessarily seem abnormal. However, in the context of "neighboring leads" (ie, the fact that the T wave in neighboring leads V3 and V4 is clearly abnormal) — I thought the T wave in lead V5 was also more voluminous than-it-should-be, given the small amplitude of the R wave in this lead.
- PEARL #2: As noted above (under assessment of R Wave Progression) — there are signs that suggest the lead V2 electrode may be malpositioned. The reason this is important — is that placement of the V1 and V2 electrodes 1 or 2 interspaces too high on the chest might be the reason why hyperacute T waves are not seen in these leads.
In the Limb Leads:
Changes in the limb leads are subtle. That said, in the context of the clearly abnormal ST-T waves we see in several of the chest leads — I suspect these subtle inferior lead ST-T wave changes are real. Note the following:
- The ST segment in lead III is downsloping. The T wave in this lead is biphasic, with terminal positivity.
- The ST segment in lead aVF is flat (albeit neither elevated or depressed).
- The QRS complex in lead aVL is tiny — which makes assessment of the ST-T wave difficult. That said, given the tiny amplitude of the R wave in this lead — I suspect the broad base and T wave height (which equals the height of the small R wave in aVL) represents a hyperacute change.
IMPRESSION: Given the clinical history of new-onset chest pain in 60-ish year old man — one has to assume from the ECG in Figure-1 that an acute cardiac event is ongoing until proven otherwise.
- More than simply representing hyperacute T waves — the peaking and huge size of the T waves in leads V3 and V4 are consistent with deWinter-like T waves. This strongly suggests the likelihood of acute proximal LAD (Left Anterior Descending) occlusion (See Audio Pearl-1 below — and ECG Blog #183 for more on this subject).
KEY Point: The more leads that manifest ST-T wave abnormalities — the greater the likelihood that acute proximal LAD occlusion is ongoing.
- As noted above (by the concept of "neighboring" leads) — lead V5 probably manifests a continuation of the acute changes seen in leads V3 and V4.
- Correction of electrode lead placement for lead V2 (and possibly also lead V1) — might lead to extension of the area manifesting acute changes to also encompass these 2 leads.
- Finally — Adding the subtle-but-real ST-T wave abnormalities described above for leads III, aVF and aVL adds further support that these ECG findings are real.
The CASE Continues:
A 2nd ECG was done during transport of this patient to the hospital. His chest pain had decreased (but had not completely resolved) at the time ECG #2 was recorded (Figure-2).
- In view of the patient's decreased symptoms — the receiving ED (Emergency Department) physician cancelled cath activation on seeing ECG #2.
QUESTION:
- What are your thoughts on the above management?
- Do you see any changes between the 2 tracings in Figure-2?
 |
| Figure-2: Comparison of the initial ECG in this case — with a 2nd ECG obtained during transport to the hospital. The patient's chest pain was less at the time ECG #2 was done (See text). |
My THOUGHTS on Seeing ECG #2:
The KEY for accurate comparison of serial tracings — is to assess whether the frontal plane axis and chest lead placement are comparable (See Audio Pearl-46a below).
- QRS morphology and amplitude, as well as the frontal plane axis — are virtually identical in ECG #2, compared to what was seen in ECG #1. Knowing this facilitates comparison of these serial tracings — and tells us that any significant change that we see between ECG #1 and ECG #2 is likely to be real.
- Careful comparison suggests there has been no significant change in the limb leads between these 2 tracings.
- Subtle changes are seen in the chest leads. Did YOU see that subtle-but-real J-point ST depression is now seen in lead V3 of ECG #2 — whereas there was no J-point ST depression in lead V3 of ECG #1? Otherwise, the T waves in leads V3, V4 and V5 all look slightly less hyperacute (ie, slightly less tall and less voluminous) than they did in ECG #1.
Would You have Cancelled Cath Lab Activation?
Although chest pain has decreased and the hyperacute T wave changes in leads V3, V4 and V5 are slightly less in ECG #2 (compared to ECG #1 done minutes earlier) — this patient had new-onset chest pain severe enough to summon EMS to his home — and — in this clinical context, ECG #1 showed ST-T wave abnormalities in no less than 6 leads consistent with deWinter-like T waves. As per Audio Pearl-1 below and ECG Blog #183 — recognition of this clinical picture tells you there is acute proximal LAD occlusion until you prove otherwise!
- PEARL #3: In the original description by deWinter et al of this syndrome — at least 1 mm of J-point ST depression was seen in one or more of the anterior leads prior to abrupt ascent to giant peaked T waves. The fact that this J-point ST depression now is seen in lead V3 of ECG #2 (whereas it was not yet seen in ECG #1) — provides further support that we most probably are dealing with deWinter T waves (and with acute proximal LAD occlusion).
- Even IF under the BEST of circumstances, the reduced chest pain and slight ECG improvement of hyperacute T waves that was seen in ECG #2 were to indicate some degree of spontaneous reperfusion — the process of acute coronary occlusion may be stuttering, sometimes evolving through spontaneous opening followed by spontaneous reocclusion one or more times until a more stable phase is reached. For this reason — acute cath lab activation is still indicated despite the improvement in symptoms! (See Audio Pearl-39a below).
Case CONCLUSION:
As noted — cardiac cath was initially cancelled. Cardiac troponins came back markedly elevated — and cardiac cath was performed the next morning. A 95-99% thrombotic lesion was found in the proximal LAD.
=======================================
NOTE: I'm repeating the following Audio Pearls below that are relevant to today's case:
=======================================
Today’s ECG Media PEARL #1 (3:00 minutes Audio) — Reviews the concept of deWinter T waves (and the common occurrence of variations on this "theme" ).
ECG Media PEARL #35a (4:50 minutes Audio) — WHEN is a T Wave Hyperacute vs a Repolarization variant?
ECG Media PEARL #39a (4:50 minutes Audio) — Reviews the concept of Dynamic ST-T Wave Changes (and how this ECG finding can assist in determining if acute cardiac cath is indicated).
ECG Media PEARL #46a (6:35 minutes Audio) — Reviews HOW to compare Serial ECGs (ie, "Are you comparing Apples with Apples or Oranges?").
==================================
Acknowledgment: My appreciation to David Didlake and Dillon Stapp (from Texas, USA) for allowing me to use this case and these tracings.
==================================
Related ECG Blog Posts to Today’s Case:
- ECG Blog #205 — Reviews my Systematic Approach to 12-lead ECG Interpretation.
- ECG Blog #183 — Reviews the concept of de Winter T Waves (with reproduction of the illustrative Figure from the original deWinter NEJM manuscript).
- ECG Blog #222 — Reviews the concept of Dynamic ST-T wave changes, in the context of a detailed clinical case.
- ECG Blog #218 — Reviews HOW to define a T wave as being Hyperacute?
- ECG Blog #230 — Reviews HOW to compare Serial ECGs (ie, "Are you comparing Apples with Apples or Oranges?").
- ECG Blog #193 — Reviews the concept of why the term “OMI” ( = Occlusion-based MI) should replace the more familiar term STEMI — and — reviews the basics on how to predict the "culprit" artery.
- ECG Blog #194 — Reviews how to tell IF the “culprit” (ie, acutely occluded) artery has reperfused using clinical and ECG data.
- ECG Blog #115 — Shows an example of how drastically the ECG may change in as little as 8 minutes.
- See My Comment at the BOTTOM of the page in the November 4, 2018 post on Dr. Smith’s ECG Blog.
- See My Comment at the BOTTOM of the page in the March 29, 2020 post on Dr. Smith’s ECG Blog (specifically my Pearl #3).





No comments:
Post a Comment