You are shown the 12-lead ECG and long lead II rhythm strip shown in Figure-1 — but without the benefit of a history.
- This ECG tells a "story". WHAT "story" does it tell?
 |
| Figure-1: What "story" is told by this ECG? |
=======================================
NOTE #1: Some readers may prefer at this point to listen to the 3:45 minute ECG Audio PEARL before reading My Thoughts regarding the ECG in Figure-1. Feel free at any time to review to My Thoughts on this tracing (that appear below ECG MP-41a).
=======================================
Today's ECG Media PEARL #41a (3:45 minutes Audio) — Reviews HOW to recognize within seconds (!) a Mobitz I ( = AV Wenckebach) 2nd-degree AV Block in which there is ongoing Inferior STEMI.
MY Sequential Approach to the ECG in Figure-1:
There are a number of important ECG findings in this case. Although I used a Systematic Approach (as I always do) to interpret both the cardiac rhythm and the 12-lead ECG (See ECG Blog #185 and Blog #205 for details on my approach) — I did allow myself the "luxury" of about 10 seconds to take in the principal findings. KEY Point: A total of 10-15 seconds was all I needed to arrive at the probable diagnosis:
- My "eye was immediately captured" by obvious signs of inferior MI of unknown age — but most probably recent (if not acute) because: i) There are deep and wide infarction Q waves in each of the inferior leads (II, III, aVF); ii) There is still significant ST elevation in each of these leads (especially considering the lack of appreciable R wave amplitude in these same inferior leads); and, iii) There is deep, symmetric T wave inversion in each of the inferior leads.
- There are some reciprocal ST-T wave changes in lead aVL (ie, a scooped, if not slightly depressed ST segment — with a disproportionately tall T wave considering small amplitude of the R wave in aVL) — but these reciprocal changes are modest!
- In the chest leads — there is ST depression in leads V1-thru-V5, which is maximal in leads V2 and V3, with a positive "Mirror Test" (See ECG Blog #246 — including the Audio Pearl in that post). In the setting of recent inferior MI — these chest lead findings are diagnostic of associated recent posterior MI.
Taking a quick look at the long lead II rhythm strip in Figure-1:
- By the Ps, Qs & 3R Approach — the QRS is narrow — at least some P waves are present — the rhythm is not completely Regular (so the Rate varies) — but a "pattern" to the rhythm does seem to be present (ie, there are several 2-beat groups that look similar — therefore, there is group beating!).
- The PR interval for all QRS complexes that are preceded by a P wave is identical, albeit prolonged (therefore, at least those P waves are Related to neighboring QRS complexes!).
NOTE: To emphasize that it need not take more than 10-20 seconds to appreciate the above ECG findings! These findings should suggest the following:
- The infero-postero MI is most probably recent. The deep Q waves plus symmetric T wave inversion in each of the inferior leads — and — the ST depression with positive T waves in the anterior leads — look like reperfusion T wave changes, which suggest that the infarction may be "complete".
- That said — the fact that ST elevation persists in each of the inferior leads (and that significant ST depression persists in leads V2 and V3) — suggest that this cardiac event could still be ongoing. Presumably the history would clarify the time sequence of events.
- PEARL #1: As to my 5-10 second assessment of the rhythm — In the setting of a recent inferior STEMI — the finding of group beating with the same prolonged PR interval that repeats throughout the tracing — will usually turn out to be the result of some form of Wenckebach (Mobitz Type I, 2nd-Degree AV Block).
To SPEED UP Your Interpretation:
While important to be thorough and systematic in ECG interpretation — application of several PEARLS can greatly expedite your assessment.
- To Instantly Recognize Posterior MI: Become comfortable mentally applying the "Mirror Test" (See ECG Blog #246). This visual aid is based on the principle that the anterior leads provide a "mirror"-image opposite ECG picture of what transpires in the posterior wall of the left ventricle. To facilitate visualization — I've inserted a mirror-image view of the 2nd and 3rd beats from leads V2 and V3 within the RED border in Figure-2. Doesn't this mirror-image view of leads V2 and V3 resemble the Q waves, ST elevation and deep, symmetric T wave inversion that we see in the inferior leads of Figure-2? It should be clear — the upright, peaked T waves in leads V2 and V3 in this patient with recent infero-postero MI are consistent with reperfusion T waves in the posterior wall distribution.
- To Instantly Suspect Wenckebach Block: Although it is challenging to recognize, because of surprisingly low amplitude of the QRS in lead II — Attention to the pattern of regularity of the rhythm in Figure-2 can be diagnostic. Clearly — there is some irregularity to the rhythm in the long lead II rhythm strip. But as shown by the RED-arrowed brackets in Figure-2 — there clearly is a pattern to this rhythm that repeats. As per PEARL #1 (above) — much of the time when I see sinus beats with group beating in the setting of recent inferior infarction — some form of Wenckebach block is present.
 |
| Figure-2: Illustration of the concepts of the "Mirror Test" and group beating — to facilitate rapid recognition of recent posterior MI and AV Wenckebach block (See text). |
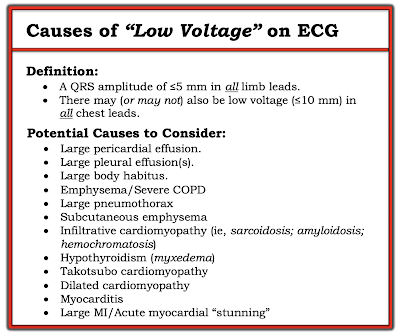
PEARL #2: Note should be made of the Low Voltage of the QRS complex, especially in the 6 limb leads.
- True Low Voltage is defined as a QRS amplitude of ≤5 mm in all limb leads. In an unselected population — true low voltage is a relatively uncommon ECG finding. Of note — there may (or may not) also be low voltage (≤10 mm) in all chest leads.
- The differential diagnosis for "low voltage" that is frequently put forth by many providers is often limited to COPD and/or pericardial effusion. As shown in Figure-3 — there are other entities to consider!
- Technically — one could dispute whether "true" low voltage criteria are met in today's ECG (because QRS amplitude in lead III may slightly exceed the 5 mm criterion). That said — overall QRS amplitude is clearly reduced in the 6 limb leads of today's tracing (as well as in most chest leads) — so the same diagnostic considerations listed in Figure-3 should still be considered.
- Of special concern in today's case — is the lack of appreciable R wave voltage in the inferior leads, as well as the small size of the R waves in leads I and aVL. Given that we were not provided with any history — the possibility of extensive infarction with myocardial "stunning" become important considerations.
 |
| Figure-3: Causes of Low Voltage (See text). |
Looking CLOSER at the Cardiac Rhythm:
At this point I wanted to gain more certainty about the cardiac rhythm. The 1st step in doing so was to determine IF the atrial rhythm was regular. I began by labeling those P waves that were clearly seen (RED arrows in Figure-4).
- Note that the PR interval before beats #2, 4, 5, 6, 7, 9, 10, 12 and 13 is the same! (ie, 0.26 second for the PR interval in front of each of these beats).
- The fact that the identical PR interval repeats tells us that each of these beats is being conducted (here with 1st-Degree AV Block).
 |
| Figure-4: I've labeled those P waves that can be clearly seen (RED arrows). |
PEARL #3: For there to be 2nd- or 3rd degree AV block — the atrial rhythm should be regular (or at least almost regular, as there may be slight R-R interval variation if an underlying sinus arrhythmia is present).
- IF this were the case — then we should look for another P wave to be found in places that fall midway between where 2 RED arrows occur close together in the long lead II rhythm strip from Figure-4.
- Setting my calipers to a P-P interval that measures precisely half the distance between the 2nd and 3rd RED arrows in Figure-4 — I found a small "extra" positive deflection in the T wave of beats #4, 5, 6, 9 and 12 (PINK arrows in Figure-5).
 |
| Figure-5: Note the small "extra" positive deflection found precisely midway between many of the RED arrows in Figure-4 (PINK arrows). |
On the theory that the underlying atrial rhythm in Figure-5 is regular — I looked for additional signs of atrial activity.
- I found I was able to "walk out" regular atrial activity throughout the entire long lead II rhythm strip (RED, PINK and PURPLE arrows in Figure-6). Note that under each of the colored arrows lies a small "extra" positive deflection consistent with regularly-occurring atrial activity.
 |
| Figure-6: Note that there are "extra" positive deflections under each of the colored arrows. Presumably — each of these colored arrows highlights the location of underlying P waves. |
The simple act of labeling P waves can be of invaluable assistance for recognizing Wenckebach conduction. For clarity — I've labeled presumed atrial activity with RED arrows in Figure-7.
- QUESTION: Is it now easier to visualize signs of Wenckebach conduction, especially for the 2-beat groups on this tracing (ie, by looking for progressive increase in the PR interval before beats #2,3; before #7,8; and before #10,11)?
 |
| Figure-7: For clarity — I've labeled all presumed P waves with RED arrows. |
Drawing the LADDERGRAM:
Now that we've established the presence of regular atrial activity — I use sequential Laddergrams in the next 5 Figures to illustrate the mechanism for the rhythm in today's case:
- As usual — I begin the laddergram in Figure-8 by drawing vertical RED lines in the Atrial Tier, directly under RED arrows in the rhythm strip to schematically show the regular occurrence of P waves (seen here at the rapid rate of 130-135/minute). The thicker BLUE arrows at the beginning of the tracing show that each of the lines in the Atrial Tier are drawn precisely under its corresponding P waves in the long lead II rhythm strip.
- I next draw arrows in the Ventricular Tier, representing conducted supraventricular beats for each of the 13 QRS complexes on this tracing (Figure-9). The thicker BLUE arrows at the beginning of the tracing show that each of the beats in the Ventricular Tier are drawn precisely under its corresponding QRS complex in the long lead II rhythm strip.
- It's now time to solve the laddergram. I do this by first connecting those atrial impulses (at the bottom of the Atrial Tier) — with those red arrows at the top of the Ventricular Tier that I know must be conducting (These are all of the beats that are preceded by an identical PR interval — as shown in Figure-10 by the BLUE slanted lines within the AV Nodal Tier).
- I continue solving the laddergram — by focusing on individual groups of beats, and connecting atrial impulses (at the bottom of the Atrial Tier) — with those red arrows at the top of the Ventricular Tier that might most logically be expected to conduct (as shown in Figure-11 by the BLUE slanted line and the 2 butt ends drawn within the AV Nodal Tier near the beginning of the tracing).
- My completed laddergram is shown in Figure-12. The rhythm is sinus (or atrial) tachycardia at ~130/minute. There is Wenckebach conduction showing a predominance of 2:1 AV conduction — and 3 2-beat groups that show 3:2 AV conduction (for beats #2,3; 7,8; and 10,11).
 |
| Figure-8: |
 |
| Figure-9: |
 |
| Figure-10: |
 |
| Figure-11: |
 |
| Figure-12: |
==================================
The "Story" that Today's ECG Tells?
Today's case was presented in the form of the 12-lead ECG and long lead II rhythm strip shown in Figure-1, without the benefit of any history.
- The 12-lead ECG indicates the occurrence of an infero-postero MI of uncertain age, but probably recent. The very deep inferior Q waves + reperfusion T waves in the inferior and anterior leads suggest that the onset of this MI is probably more than a couple of hours old — although persistent inferior ST elevation and anterior ST depression indicate that the event may still be ongoing.
- The underlying rhythm is atrial (or sinus) tachycardia, with group beating due to Wenckebach conduction.
- 2nd-Degree AV Block, Mobitz Type I (ie, AV Wenckebach) — is a common accompaniment of acute or recent inferior infarction. Most of the time this conduction disturbance does not require cardiac pacing.
- The low voltage, predominant inferior Q waves (with negligible R wave amplitude in these leads), and the rapid atrial rate all raise concern for the possibility of cardiac decompensation.
==================================
Acknowledgment: My appreciation to Kianseng Ng (from Malaysia) for making me aware of this case and allowing me to use this tracing.
==================================
Relevant ECG Posts to Today's Case:
- ECG Blog #185 — Use of a Systematic Approach to Rhythm Interpretation.
- ECG Blog #205 — Reviews my Systematic Approach to 12-lead ECG Interpretation.
- ECG Blog #246 — Review use of the "Mirror Test" for the diagnosis of acute posterior MI.
- ECG Blog #258 — Reviews HOW to "Date" an Infarction.
- ECG Blog #184 — Reviews the "magical" mirror-image opposite relationship with acute ischemia between lead III and lead aVL.
- ECG Blog #55 — Acute inferior MI + AV Wenckebach.
- ECG Blog #154 — Acute inferior MI + AV Wenckebach.
- ECG Blog #168 — Acute inferior MI + Wenckebach (dual-level) block.
- ECG Blog #224 — Acute inferior MI + AV Wenckebach.
- ECG Blog #188 — How to Read (and Draw) Laddergrams.
- The January 24, 2020 post in Dr. Smith's ECG Blog — Reviews a case in which Low Voltage (with progressive reduction in QRS amplitude on serial ECGs) was due to myocardial stunning (See My Comment at the bottom of the page).
- The November 12, 2020 post in Dr. Smith's ECG Blog — Reviews a case in which Low Voltage was seen in a patient with Covid-19 and cardiogenic shock (See My Comment at the bottom of the page).


I read this again! Amazing! And I did read your comments in Dr Smith's Bog on Low QRS voltage. I saw this, "This has been a great blog, but has grown more valuable since Dr Grauer´s section was incorporated. A must read. THANKS FROM Venezuela", I echo the Venezuelan Doctor's comments, certainly Prof KG enriches everyone, everywhere, each time he speaks and he speaks with Everest Authority!
ReplyDeleteThank you so much for your kind words! My please — :)
Delete