The ECG in Figure-1 was obtained from a patient with new chest pain. He was hemodynamically stable at the time this tracing was obtained.
- How would you interpret the rhythm and, the rest of this ECG?
- NOTE: In addition to the artifact that is most pronounced in the lateral chest leads — there are 4 Major Findings. Two of these findings are admittedly subtle. How many of these 4 findings can you identify?
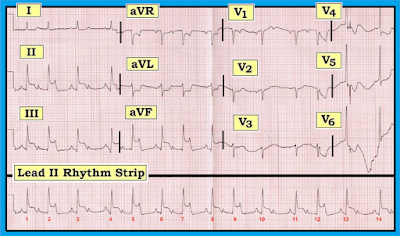 |
| Figure-1: ECG obtained from a patient with new chest pain. Can you identify the 4 Major Findings on this tracing? |
Interpretation: As always, once we ensure that the patient is hemodynamically stable — We begin our Systematic Approach with assessment of the Rate & Rhythm.
COMMENT: We suspect the “culprit artery” in this case is acute occlusion of the RCA (Right Coronary Artery) — because: i) In ~80-90% of patients — there is a dominant RCA circulation, which means that most acute inferior MIs are due to acute occlusion of the RCA instead of the LCx (Left Circumflex Artery); ii) The amount of ST elevation in lead III is > lead II (the opposite tends to be true with acute LCx occlusion); and, iii) There is a significant amount of reciprocal ST depression in lead aVL (this is less likely to be seen with acute LCx occlusion).
-------------------------------------------------------------------------
- Rate & Rhythm —The rhythm in this tracing is complex — so we will defer full interpretation for a few moments. As we will see shortly, it is clinically useful in this case to delay detailed rhythm analysis — because one of the biggest hints for interpreting this rhythm lies in what we find in the rest of the 12-lead ECG!
- What is obvious about the rhythm — is that the ventricular rhythm is fairly fast — that there is atrial activity — and, that as we step back a bit from the tracing, there is a repetitive pattern = group beating. That is, there are groups of 2 beats and occasionally just 1 beat. That this is not due to chance should be evident because the distance after the 2-beat groups until the next group begins is always the same! (ie, the R-R interval between beats #2-3; between #5-6; between #7-8; 9-10; and 12-13 is the same)! Similarly, the distance after the 1-beat groups until the next group begins is also the same! (ie, the R-R interval between beats #3-4; between #10-11; and between #13-14 is the same)!
- PEARL #1: The presence of group beating should always make you consider the possibility of some type of Wenckebach block.
- At this point in the interpretation process — We suggest deferring further assessment of the cardiac rhythm until after you have looked at the rest of the 12-lead ECG. After all, this patient presented with new-onset chest pain — and even before scrutinizing the “details”, it looks like something acute is going on! Continuing with our Systematic Approach — We note the following:
- Intervals —The PR interval appears to be changing — although it is useful to note that the PR interval is constant and normal at the onset of each of the small groups in this tracing (ie, the PR interval before beats #1, 3, 4, 6, 8, 10, 11, 13 and 14 is normal and equal)! The QRS complex is normal (ie, not more than half a large box in duration) — therefore, this is a supraventricular rhythm. The QT interval does not appear to be prolonged — although the irregular rate makes this challenging to assess.
- Axis —The frontal plane axis is normal (approximately +75 degrees).
- Chamber Enlargement — P waves are peaked in each of the inferior leads — but not quite tall enough to qualify for RAA (Right Atrial Abnormality), since P waves are less than half a large box tall. There is a fairly deep negative component to the P wave in lead V1 — which qualifies for LAA (Left Atrial Abnormality). Of note — LVH (Left Ventricular Hypertrophy) is probably present! Although neither of the 2 most common voltage criteria for LVH are satisfied in this tracing (ie, deepest S in V1,V2 + taller R in V5,V6 ≥35mm – or – R in aVL ≥12mm) — voltage criteria for LVH are satisfied in lead V6 (R in V6 ≥18-20mm). And although there clearly is much baseline wander + artifact in leads V4-thru-V6 — the ST-T waves in these leads suggests there may be LV “strain”. Recognition of probable LVH in this tracing is the 1st of the 4 major findings that are present. We suspect many observers may overlook this finding.
- Q-R-S-T Changes —There are small q waves in each of the inferior leads. In addition, leads II, III and aVF clearly show ST elevation (of at least 3-4mm) — which occurs in association with reciprocal ST depressionin lead aVL. In a patient with new chest pain — these limb lead findings are diagnostic of an acute inferior STEMI, which is the 2nd of the 4 major findings on this ECG. Otherwise — transition occurs normally in this tracing (ie, the R wave becomes taller than the S wave is deep between leads V3-to-V4). And although a QS complex is seen in leads V1 and V2 — a small-but-definite initial r wave is seen in lead V3. We therefore doubt this patient has had prior anterior infarction. Instead, we suspect the presence of LVH accounts for the lack of initial r wave in V1, V2.
COMMENT: We suspect the “culprit artery” in this case is acute occlusion of the RCA (Right Coronary Artery) — because: i) In ~80-90% of patients — there is a dominant RCA circulation, which means that most acute inferior MIs are due to acute occlusion of the RCA instead of the LCx (Left Circumflex Artery); ii) The amount of ST elevation in lead III is > lead II (the opposite tends to be true with acute LCx occlusion); and, iii) There is a significant amount of reciprocal ST depression in lead aVL (this is less likely to be seen with acute LCx occlusion).
-------------------------------------------------------------------------
QUESTION: Most of the time with acute inferior STEMI — there will be ST depression in anterior leads due to associated acute posterior involvement.
- What might be the reason why there is virtually NO anterior ST depression in leads V1, V2 or V3 of Figure-1?
- In patients with marked LVH + “strain” — the anterior leads often show the opposite (mirror-image) picture of ST-T wave changes as are seen in lateral chest leads. We illustrate this in Figure-2 — taken from our ECG Blog #73 on ECG criteria for LVH.
- Return to the ECG in Figure-1. It is rare to see nearly flat ST-T waves in the anterior leads of a patient with as much inferior ST elevation as occurs in Figure-1. As the 3rd major finding in this case — we suspect there is associated acute posterior MI in this case. Given the presence of LV “strain” in V5, V6 — the baseline tracing of this patient most probably manifested prominent upright ST-T waves in the anterior leads (similar to those seen in leads V2 and V3 in Figure-2). As a result, with acute occlusion of the RCA — there was acute infero-postero STEMI that probably produced anterior ST depression, which we suspect was attenuated by the prominent upright ST-T waves that are so commonly seen in anterior leads of patients with LVH.
-------------------------------------------------------------------------
Returning to the RHYTHM in this Case: We have just diagnosed acute inferior STEMI (most probably with associated acute posterior involvement) — that is probably the result of acute RCA occlusion.
Returning to the RHYTHM in this Case: We have just diagnosed acute inferior STEMI (most probably with associated acute posterior involvement) — that is probably the result of acute RCA occlusion.
- PEARL #2: Whenever you see group beating in a patient with acute inferior STEMI — the chances are excellent that 2nd-Degree AV Block, Mobitz Type I (= AV Wenckebach) is the cause of the group beating! Awareness of this clinical reality greatly facilitates a more careful analysis of the rhythm.
- Beyond-the-Core: It is especially likely that the cause of group beating with acute inferior MI is AV Wenckebach when noneof the R-R intervals are longer than twice the shortest R-R interval on the tracing!
- For clarity — we outline groups of beats in the long lead II Rhythm Strip. Dotted BLACK rectangles highlight groups of 2 beats — and dotted RED rectangles highlight groups of 1 beat (Panel A in Figure-3). As noted earlier — we KNOW this represents true “group beating” — because all 2-beat groups are similar to each other, and all 1-beat groups similar.
- PEARL #3: The simple step of using calipers and labeling P waves is always amazingly helpful to me in facilitating my recognition of complex arrhythmias. To determine IF the underlying atrial rhythm is regular — I start with an R-R interval within which I can see 2 P waves. This tells me what the P-P interval will be (ie, the distance between the first 2 RED arrows in Panel B of Figure 3). Set your calipers precisely to this distance — and see if you can walk out regular atrial activity throughout the tracing. RED arrows in Figure-3 show that we can!
- We have already noted that the PR interval is constant and normal at the onset of each of the small groups in this tracing (ie, the PR interval before beats #1, 3, 4, 6, 8, 10, 11, 13 and 14 is normal and equal). This tells us that there IS conduction!
- IF we now focus our attention within the groups of 2 beats (ie, within the dotted BLACK rectangles) — it should be apparent that the PR interval increases until a beat is dropped. For example — the PR interval preceding beat #5 is longer than the PR interval preceding beat #4 — and then the next P wave (which occurs within, and which peaks the T wave of beat #5) is nonconducted. The cycle then begins again with shortening of the PR interval that precedes beat #6.
- The rhythm is therefore 2nd-Degree AV Block, Mobitz Type I (= AV Wenckebach), with alternating 3:2 and 2:1 AV conduction. We determine these conduction ratios on the basis that for groups within the BLACK rectangles — there are 3 P waves, but only 2 of them are conducting (ie, 3:2 AV conduction). And, within the RED rectangles — there are 2 P waves, but only 1 of them conducts (ie, 2:1 AV conduction). NOTE: The rhythm is the 4th major finding in this case!
 |
| Figure-3: Labeling of Figure-1 to illustrate the presence of 1-beat and 2-beat groups (Panel A). In Panel B — RED arrows illustrate the presence of a regular underlying sinus rhythm (See text). |
-------------------------------------------------------------------------
LADDERGRAM Illustration of the Rhythm: We conclude this blog post with a laddergram of the rhythm (Figure-4). While construction of laddergrams can be quite complex when the rhythm is challenging — we emphasize that readinga laddergram that has already been constructed for you is EASY.
LADDERGRAM Illustration of the Rhythm: We conclude this blog post with a laddergram of the rhythm (Figure-4). While construction of laddergrams can be quite complex when the rhythm is challenging — we emphasize that readinga laddergram that has already been constructed for you is EASY.
- Vertical RED lines in Figure-4 show the underlying regular atrial rate. Note that each vertical line in the Atrial Tier lies directly under its corresponding P wave in the long lead II rhythm strip.
- Focus your attention next on the Ventricular Tier. Each line with an arrow corresponds to conduction of a QRS complex through the ventricles.
- Finally — See how the middle = AV Nodal Tier illustrates the Wenckebach mechanism. Within each of the 2-beat groups (ie, beats #1-2; 4-5; 6-7; 8-9; and 11-12) — the degree of slanting increases. This corresponds to progressive lengthening of the PR interval within a group until a beat is dropped — and then, the PR interval shortens (the amount of slanting decreases) as the next cycle begins.
 |
| Figure-4: Laddergram illustration of Figure-3 (See text). |
-------------------------------------------------------------------------
SUMMARY of this CASE: This is indeed a challenging ECG to interpret — with 4 major findings: i) acute inferior STEMI; ii) probable LVH with “strain”; iii) probable associated acute posterior infarction; and iv) 2nd-Degree AV Block, Mobitz Type I ( = AV Wenckebach), with alternating 3:2 and 2:1 AV conduction.
- The 2 most important findings to appreciate are interpretation of the cardiac rhythm, and recognition of the acute STEMI. Extra Credit to you if you picked up on LVH and the associated posterior infarction.
- Among the most important “Take-Home” Points of this case are learning how to recognize the phenomenon of group beating — and, realizing that once you see true group beating in the setting of acute inferior STEMI — the most likely etiology of the rhythm will be Mobitz I. With practice — this should literally take no more than a handful of seconds to recognize! You can then verify that Mobitz I is truly the etiology of the rhythm by: i) Using your calipers to verify that regular P waves are present; and, then ii) Focusing your attention within each group of beats to see if the PR interval progressively lengthens until a beat is dropped — before then restarting the next cycle with a shortened PR interval.
- CHALLENGE: Test your newly acquired skill by interpreting the 12-lead ECG and rhythm strip shown in Figure-5. Detailed assessment of this tracing is explained (and illustrated with laddergram) in our ECG Blog #55.
 |
| Figure-5: 12-lead ECG and long lead II rhythm strip obtained from a 50-year-old woman with chest pain. What is going on? What is the rhythm? Detailed answers appear in our ECG Blog #55. |
-------------------------------------------------------------------------
Acknowledgment: My thanks to Gëzim Berisha from Kosovo-Prishtina, for his permission allowing me to use this tracing and clinical case.
-------------------------------------------------------------------------
Acknowledgment: My thanks to Gëzim Berisha from Kosovo-Prishtina, for his permission allowing me to use this tracing and clinical case.
-------------------------------------------------------------------------
-------------------------------------------------------------------------
NOTE: The following blogs and reference materials provide more information on topics mentioned in this case:
- Our 1-hour ECG Video on the Basics of AV Block = EASY LINK = www.avblockecg.com — NOTE: If you click on SHOW MORE (on the YouTube page, under the video) — you’ll see a detailed linked Contents that will facilitate quickly finding whichever part of this video you will to review!
- Our suggested Systematic Approach to 12-Lead ECG Interpretation — See ECG Blog #93.
- Step-by-Step illustration of HOW to Draw Laddergrams — See ECG Blog #69.
- Here are a few cases of Acute MI + AV Block — See ECG Blog #48 and Blog #55.
- Click HERE — For free Download of our Section 20 (from ACLS-2013-ePub) on AV Block/AV Dissociation.
- Review of ECG Criteria for Atrial Abnormality (in ECG Blog #75) — and for LVH (in Blog #73).




