The ECG in Figure-1 was obtained from a 35-year old man with a 20-pack year history of smoking — who presented with new-onset chest discomfort. He was hemodynamically stable at the time this tracing was obtained.
- How would you interpret his ECG?
- Is there RBBB?
- Should the cath lab be activated?
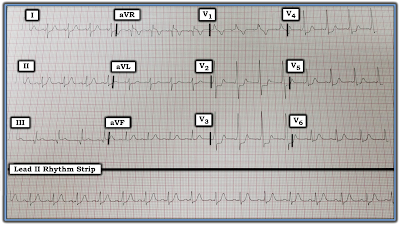 |
| Figure-1: ECG obtained from a 35-year old man with new-onset chest discomfort. Should the cath lab be activated? |
=============================
Interpretation: There is a regular sinus rhythm in Figure-1 at a rate of ~90/minute. At first glance, the PR interval looks normal — but the QRS complex looks wide, with a pattern in lead V1 that suggests RBBB (Right Bundle Branch Block). That said, this is not RBBB. Why not?
=============================
ANSWER: The pattern of QRS widening with the upright complex in lead V1 is not the result of RBBB. The reason for this is highlighted by the RED arrows in Figure-2, which point to delta waves that are evident in leads I and V2-thru-V5. This patient has WPW (Wolff-Parkinson-White) Syndrome.
- Delta waves are not obvious in a number of leads on this tracing. This is especially true in several of the limb leads. It was only after I saw unmistakable slurring of the initial part of the QRS complex in certain leads (most evident in leads V2, V3 and V4) — that I realized this patient has WPW.
- PEARL #1: Delta waves are not always seen in all 12 leads of the ECG when a patient has WPW. As a result, it can sometimes be quite challenging to make the diagnosis. This problem is complicated by the reality that some patients (more common in older individuals) normally manifest some initial slowing (and therefore slurring) of the early part of the QRS complex. BOTTOM LINE: When contemplating the possibility of WPW — all 12 leads should be carefully scrutinized. If questionable initial slurring is minimal and only noted in 1 or 2 leads — then the patient probably does not have WPW. But if unmistakable delta waves associated with a short PR interval are definitely seen (as is highlighted by the RED arrows in leads V2, V3 and V4 of Figure-2) — then you have made your diagnosis despite the absence of obvious delta waves in some of the other leads.
- PEARL #2: Once you determine the patient has WPW — you’ll often be able to GO BACK and recognize subtle deflections that in retrospect are also delta waves. For example, in Figure-2 — I initially thought there was a Q wave in lead III (WHITE arrow). However, the fact that this negative deflection in lead III occurs at precisely the same instant in time as the delta wave in simultaneously-obtained lead I (dotted WHITE line, leading up to the RED arrow in lead I) — tells us that this negative deflection in lead III is actually a negative delta wave.
- This illustrates why WPW is often referred to as, “the great ECG mimic” — because WPW may simulate a number of ECG findings, including myocardial infarction (if there are multiple negative delta waves), as well as chamber enlargement, ischemia, and conduction defects! Thus, there is no RBBB in Figure-2 — because this patient has WPW.
- Other examples of “retrospective recognition” of delta waves in Figure-2 are seen in leads II, aVL, and aVF. Thus, the suggestion of a tiny “extra little bump” on the baseline in leads II and aVF probably represents subtle delta waves that are almost entirely isoelectric.
=============================
ECG Findings with WPW: When the rhythm is sinus — conduction of the electrical impulse in a patient with WPW begins as usual in the SA node. From there, the impulse may be conducted to the ventricles in one of 3 ways:
- Possibility #1: Entirely over the AP (Accessory Pathway) — in which case the AV node will be completely “bypassed”, resulting in: i) a delta wave (due to slow conduction through nonspecialized myocardial tissue); ii) a short PR interval (since the usual delay in conduction inherent within the AV node is bypassed); and, iii) a wide QRS complex (from slowed conduction through the ventricles) — OR —
- Possibility #2: Conduction to the ventricles with WPW may at times be entirely over the normal AV nodal pathway (in which case there will be no delta waves on the ECG; the PR interval will be normal; and the QRS complex will be narrow and look normal) — OR —
- Possibility #3: There may be simultaneous conduction over both the AP and the normal AV nodal pathway! If relatively more conduction occurs over the AP — then the QRS complex will be wide, and there will be delta waves and a short PR interval. If instead, preexcitation is limited so that conduction occurs primarily over the normal AV nodal pathway — then the features of WPW may be subtle, and you may not even realize that an AP exists. But, if a significant amount of conduction is simultaneously transmitted over both the AP and the normal AV nodal pathway — then the resultant PR interval and QRS complex may reflect features intermediate between normal and preexcited complexes.
=============================
NOTE: For more on the ECG features of WPW, as well as clinical implications when WPW is found in an asymptomatic patient — Please see our ECG Blog #153.
=============================
QUESTION: What about the marked ST segment depression seen within the WHITE rectangles in Figure-2 (BLUE arrows)? Is this ST depression that is seen in most chest leads reflective of ischemia in this 35-year old man with new chest discomfort? — OR — Are we unable to assess the significance of this finding because this patient has WPW?
- KEY POINT: In general — assessment of ST-T wave deviations (elevation or depression) do not reliably predict underlying ischemia or infarction when there is considerable preexcitation. This is because since the sequence of depolarization is altered by WPW — the sequence of repolarization (and therefore the appearance of ST-T waves) will also be altered. That said, the shape and amount of ST depression within the WHITE rectangles in Figure-2 is so pronounced — that one wonders if despite the presence of WPW, this ST depression might nevertheless indicate acute ischemia?
=============================
Follow-Up: The cardiologist involved in the case was as uncertain as I am looking at this ST depression (within the WHITE rectangles) — as to whether it is a marker of acute ischemia, or simply an accompaniment of this patient’s WPW. Given this patient’s history ( = risk factors + new-onset chest pain) — cardiac catheterization was performed. The coronary arteries were free of significant disease.
-------------------------------------------------------------------------
COMMENT: Most of the time, you will not be able to appreciate ischemia or acute infarction on the ECG of a patient with WPW. That said, on occasion — ST-T wave changes may be so marked as to suggest acute disease, necessitating cardiac cath to define the anatomy. This was the situation in this case.
-------------------------------------------------------------------------
Acknowledgment: My thanks to Dr. Ahmed Abbas from Amman, Jordan, for his permission allowing me to use this tracing and clinical case.
-------------------------------------------------------------------------
-------------------------------------------------------------------------
- NOTE: For more on the ECG features of WPW, as well as clinical implications when WPW is found in an asymptomatic patient — Please see our ECG Blog #153.
- CLICK HERE — for a link to Dr. Stephen Smith's ECG Blog post from March 1, 2012, in which he shows a series of WPW tracings which either mimic, hide or reveal acute MI.


What about ablation of preexcitation pathway?
ReplyDeleteSORRY for my delay in answering! Good question you ask. Unfortunately, I don't know if ablation was done ...
DeleteI wouldn't have identified the pre-excitation on this ekg, but with more obvious pre-excitation (or with more expert interpretation than mine) could smith-modofied sgrabossa be helpful given the abnormal ventricular conduction? Looking at this tracing it seems some leads come close to meeting the criteria (most notably I/avr) but i don't think any are definitively positive
ReplyDeleteSORRY for my delay in answering! First — with practice, my hope is that you'll better recognize WPW in cases like this one. Otherwise, while I consider Smith-Sgarbossa criteria — my bias/preference has ALWAYS been qualitative review of the entire tracing. In cases like this one — I look for ST elevation or depression that "shouldn't be there". I explain that this IS present in this tracing. I do NOT believe ( = my opinion) that there is data to "scientifically assess" Sgarbossa-like criteria on ALL of the too-many-to-count potential variants of QRST morphology — so for me ( = my opinion) — Sgarbossa-like criteria are not helpful in this case. Hope that addresses your question — :)
Delete