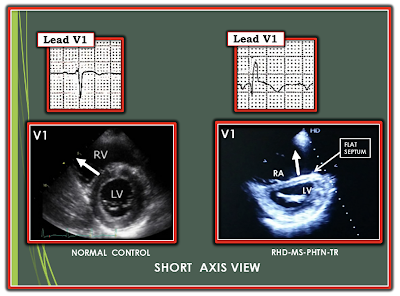
The 2 ECGs shown in Figure-1 are both of patients from India, who share a similar pathologic process. Describe the valvular pathology they share. Be as specific as possible!
Extra Credit:
- What additional information does the QRS morphology in lead V1 suggest?
 |
| Figure-1: ECGs of 2 patients from India who share a similar pathology. Can you guess the valvular pathology that they share? |
=======================================
NOTE: Some readers may prefer at this point to listen to the 9:00-minute ECG Audio PEARL before reading My Thoughts regarding the ECG in Figure-1. Feel free at any time to refer to My Thoughts on this tracing (that appear below ECG MP-62).
=======================================
Today's ECG Media PEARL #62 (9:00 minutes Audio) — Reviews my LIST #6: Common Causes of a Tall R Wave in Lead V1.
- NOTE: I review the concepts put forth in today's Audio Pearl in ECG Blog #81.
MY Thoughts on the 2 ECGs in Figure-1:
As always — I favor the use of a Systematic Approach (which I review in ECG Blog #205):
ECG #1:
- The rhythm is sinus at 80-85/minute. Regarding intervals — the PR interval and QRS duration are both upper normal (ie, 0.20 second and 0.10 second, respectively). The QTc looks to be borderline prolonged. There is marked RAD (Right Axis Deviation) — in that the QRS complex in lead I is predominantly negative.
- Regarding Chamber Enlargement — there is RAA = Right Atrial Abnormality (very tall, peaked P waves in lead II) — LAA = Left Atrial Abnormality (very deep and wide negative P wave in lead V1) — and RVH = Right Ventricular Hypertrophy (marked RAD, RAA, predominant R wave in lead V1; ST-T wave changes consistent with RV "strain" — and — persistent deep S waves in the chest leads through to lead V6).
- Regarding Q-R-S-T Changes: As is common (and not unusual) — there is a Q wave in lead aVR. But an important finding is the small-but-real Q wave in lead V1 (as well as the tiny q wave in lead V2). I've already noted the predominant R wave in lead V1 — as well as the finding of RV "Strain" (ST-T depression in both inferior and anterior leads).
ECG #2:
- The rhythm AFib (Atrial Fibrillation) with a controlled ventricular response (ie, irregularly irregular rhythm without any P waves — within a ventricular rate range begtween ~65-to-100/minute). Regarding intervals — there is no PR interval (No P waves); the QRS is narrow and the QTc is normal.
- There is marked RAD (ie, predominantly negative QRS complex in lead I).
- Regarding Chamber Enlargement — there is RVH (marked RAD, predominant R wave in lead V1; — and persistent S waves through to lead V6).
- Regarding Q-R-S-T Changes: There is a qR pattern in lead V1. R wave progression normalizes after this predominant R wave in lead V1. There is nonspecific ST-T wave flattening in virtually all leads — but clearly no acute changes.
==============================
Clinical PEARLS regarding ECGs #1 and #2:
Although there are definite differences in the ECG findings seen in the 2 tracings shown in Figure-1 — both ECGs share a common pathophysiology. As a result — I'll synthesize my observations in the form of a series of clinical PEARLS regarding interpretation of these 2 tracings.
- The principal ECG finding in both tracings is marked RVH. As emphasized many times in this ECG Blog (See ECG Blog #234) — I favor thinking of RVH as a "detective" diagnosis — in that no single ECG criterion by itself can reliably diagnose RVH. Instead, a combination of ECG findings is needed. This is emphatically illustrated in ECG #1 — in which criteria supporting the ECG diagnosis of RVH include the following: i) marked RAD; ii) RAA; iii) predominant R wave in lead V1; iv) RV "strain" in both inferior and anterior leads; and, v) deep persistent S waves through to lead V6.
NOTE: One might be tempted to interpret the findings in ECG #1 as consistent with anterior ischemia and infarction — because there are Q waves in leads V1 and V2 — QRS morphology in leads I, V1 and V6 is consistent with IRBBB (Incomplete RBBB) — and — there is ST-T depression in the inferior and anterior leads (which is marked in leads V3 and V4).
- PEARL: The "tip-off" that something other than acute ischemic heart disease is operative is the huge size of the P waves in leads II and V1!
- As emphasized in ECG Blog #75 — the finding of large (ie, ≥2.5 mm) and pointed P waves that "look uncomfortable to sit on" in one or more of the inferior leads indicates RAA (and the huge P wave in lead II of ECG #1 is 3-4 mm tall! ).
- KEY Point: There is only 1 condition in medicine that produces right atrial enlargement without also producing RVH. That condition is tricuspid stenosis, which is rare. Therefore, the ECG finding of RAA that is not the result of slender body habitus — often provides an important indirect clue to the presence of RVH.
- The depth and width of the negative P wave in lead V1 is about as deep as you will ever see! Whether due to true left atrial enlargement — or, dramatically increased left atrial pressure — or, a huge right atrium that "flops over", producing this huge negative P wave component in lead V1 — the point to emphasize is that something other than simple acute ischemic heart disease is likely to be operative!
- PEARL: Another "tip-off" that something other than acute ischemic heart disease is operative is that despite lack of QRS widening (ie, no RBBB) — there is a Tall R Wave in lead V1 — which as per the Audio Pearl in today's blog post (above), suggests a differential diagnosis with strong consideration of RVH as the cause.
NOTE: The fact that we are told that the 2 patients in today's case share a common pathophysiology — and — that both of these patients come from India provides 2 important clues to the common pathophysiology that these patients share:
- Although the abnormal findings in ECG #2 are fewer and less dramatic — they are even more suggestive of the shared pathophysiology in today's case than was ECG #1. Once again, ECG #2 is diagnostic of marked RVH because there is: i) marked RAD (predominantly negative QRS in lead I); and, ii) a narrow QRS complex with a small-but-nevertheless predominant R wave in lead V1. As emphasized in ECG Blog #234 — by the time one sees a predominant R wave in lead V1 in an adult, the degree of RVH is marked. This is especially true when the degree of RAD is as extreme as is suggested by the predominantly negative QRS complex seen in lead I of ECG #2.
- The 3rd important finding in ECG #2 is the small-but-real initial negative deflection (q wave) for the QRS complex in lead V1, which makes for a "qR" pattern. The presence of a qR pattern in lead V1 in a patient with RVH is a marker of severe pulmonary hypertension, with increased risk of mortality (Waligóra et al: J Electrocardiol — 50(4): 476-483, 2017).
- The 4th important finding in ECG #2 is AFib (irregularly irregular rhythm without P waves) — because this completes a clinical Triad (AFib + RVH + qR in V1) that strongly suggests RHD (Rheumatic Heart Disease) with severe MS (Mitral Stenosis) and resultant pulmonary hypertension until you prove otherwise! This is because as mitral stenosis progresses (and mitral valve area decreases) — left atrial size (and resultant LA pressure) progressively increase — with proportional increase in pulmonary arterial and venous pressures. Clinical decompensation may rapidly occur once AFib develops, as this eliminates the "atrial kick" which had provided important enhancement of left ventricular filling that the patient depended on (CLICK HERE for an excellent review in the Cardiology Advisor by O'Gara & Udell on the diagnosis and clinical features of Mitral Stenosis).
WHY is it Helpful to Know that Both Patients are from India?
Because my clinical practice was in the United States — the number of patients with RHD (Rheumatic Heart Disease) that I saw during my career was extremely limited.
- Overall (presumably as a result of widespread antibiotic use) — the incidence of RHD in developed countries has dramatically decreased over the past century. Currently — the estimated prevalence of RHD in developed nations is ~1/100,000.
- In contrast — the prevalence of RHD (with potentially significant valvular sequelae) remains much higher in those crowded areas of less developed nations. For example — the estimated prevalence of RHD in India is ~100-150 cases/100,000 population, which is over 100-fold increased compared to the prevalence of RHD in developed countries (Medscape — Shah and Sharma — and Seckeler and Hoke).
- Bottom Line for Today's Case: The ECG finding of marked RVH in association with presumed pulmonary hypertension (ie, qR pattern in lead V1) — especially in association with AFib — in a patient from a country with a high prevalence of RHD should immediately suggest severe mitral stenosis from advanced RHD as the cause.
2 Final Points regarding the qR Pattern in Lead V1:
- Technically — one might be tempted to call the qR pattern that we see in lead V1 of both ECGs as consistent with IRBBB (Incomplete RBBB) — because terminal S waves are seen in lateral leads I and V6 of both tracings. My preference (given the totality of ECG findings) — is to attriubte this qR pattern to severe RVH with pulmonary hypertension, rather than to postulate a conduction defect. That said — it is true that complete and/or incomplete RBBB is a common accompaniment of RVH (and I would completely accept an interpretation of RVH plus IRBBB).
- There is a physiologic reason why pulmonary hypertension from advanced mitral stenosis commonly results in a qR pattern in lead V1 (Figure-2).
In Conclusion: Both of the patients in today's case shared a common pathophysiology:
- Both patients had RHD, with resultant severe mitral stenosis + pulmonary hypertension + RV dilatation with severe tricuspid regurgitation.
- This pathophysiology is easily predictable by the fact that: i) Both patients come from a country with a high prevalence of RHD (ie, they are both from India); and, ii) The ECG of each patient shows marked RVH with a qR pattern in lead V1 — as well as other ECG findings consistent with severe mitral stenosis (ie, AFib, RAA, LAA).
==================================
Acknowledgment: My appreciation to Dr. R Balasubramanian (from Pondicherry, India) for allowing me to use this case and these tracings.
==================================
Related ECG Blog Posts to Today’s Case:
- ECG Blog #205 — Reviews my Systematic Approach to 12-lead ECG Interpretation.
- ECG Blog #81 — Reviews the List of Common Causes of a Tall R Wave in Lead V1 — including KEY points for detection of each of the 6 causes in our List.
- ECG Blog #234 — My updated version on the ECG diagnosis of RVH (Listen to the 7-minute Audio on RVH in this post = ECG Media Pearl #50).
- ECG Blog #77 — My original discussion on the ECG criteria for RVH.
- ECG Blog #75 — Reviews "My Take" on the ECG criteria for RAA & LAA.
- ECG Blog #156 — Reviews the case of an adult with uncorrected Tetraology of Fallot (with marked RVH + pulmonary hypertension).
- ECG Blog #204 — Reviews "My Take" on the ECG diagnosis of the Bundle Branch Blocks (See the 13-minute Video in this post = ECG Media Pearl #22).
- ECG Blog #193 — illustrates use of the Mirror Test to facilitate recognition of acute Posterior MI. This blog post reviews the basics for predicting the "culprit artery". NOTE: Figure-5 in the Addendum of this blog post illustrates the essentials for identifying an isolated posterior MI.
- ECG Blog #80 — reviews prediction of the "culprit" artery (and provides another case illustrating the Mirror Test for diagnosis of acute Posterior MI).
- The September 1, 2020 post in Dr. Smith's ECG Blog — My Comment (at the bottom of the page) reviews the case of a young woman with Primary Pulmonary Hypertension (which is diagnosable from the ECG! ).
- The September 21, 2020 post in Dr. Smith's ECG Blog — My Comment (at the bottom of the page) emphasizes utility of the Mirror Test for diagnosis of acute Posterior MI.
- The February 16, 2019 post in Dr. Smith's ECG Blog — My Comment (at the bottom of the page) emphasizes utility of the Mirror Test for diagnosis of acute Posterior MI.



No comments:
Post a Comment