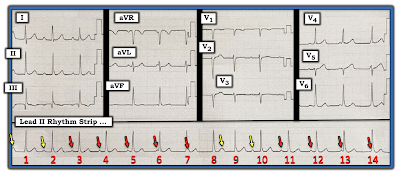
The ECG in Figure-1 was obtained as part of a routine exam of an otherwise healthy and asymptomatic 30-year old man.
QUESTIONS:
- What are the abnormal findings in Figure-1?
- Are any of the P waves conducted to the ventricles?
- Clinically — HOW should this patient be treated?
 |
| Figure-1: ECG obtained from an otherwise healthy and asymptomatic 30-year old man. Can you explain the abnormal findings? |
=======================================
NOTE: Some readers may prefer at this point to listen to the 5:45-minute ECG Audio PEARL before reading My Thoughts regarding the ECG in Figure-1. Feel free at any time to refer to My Thoughts on this tracing (that appear below ECG MP-61).
=======================================
Today's ECG Media PEARL #61 (5:45 minutes Audio) — Reviews HOW to Tell IF a P Wave is Conducting? Being able to answer this question is KEY for determining the etiology of complicated AV Block/AV Dissociation tracings.
MY Sequential Thoughts on the ECG in Figure-1:
As always — I favor the use of a Systematic Approach for interpreting ECG findings in the 12-lead (which I review in ECG Blog #205) — and — the Ps, Qs & 3Rs Approach for initial assessment of the cardiac rhythm, especially when the rhythm is complicated (as reviewed in ECG Blog #185).
- My initial impression of the rhythm, as seen in the long lead II rhythm strip in Figure-1 — was that the QRS complex was narrow — that fairly regular P waves were seen — that the ventricular rhythm was for the most part regular (at a rate of ~80-85/minute) — and, that most of the P waves looked to be conducting. And then I noticed that the PR interval was decreasing ... This suggested that the mechanismo of this rhythm was more complex than what I initially thought.
PEARL #1: It's fine to make a quick, initial hypothesis. The experienced clinician routinely does this in virtually all aspects of medicine — often suggesting a preliminary diagnosis to us within seconds of seeing the patient. But after this brief, almost intuitive impression — what should then follow, is a far more specific series of inquiries and assessments that either confirm or negate our initial impression.
- In the field of arrhythmia interpretation — IF your initial impression is wrong (as mine was for the rhythm in Figure-1) — GO BACK to the BASICS (which means step-by-step assessment by the Ps, Qs & 3R Approach).
- Number the beats in the rhythm strip.
- Use calipers to determine IF there are regular (or at least fairly regular) P waves throughout the rhythm strip (Figure-2).
 |
| Figure-2: I have numbered the beats in the long lead II rhythm strip from Figure-1. I then used calipers to facilitate labeling P waves throughout this tracing. |
QUESTIONS:
- Is the atrial rhythm regular (or at least almost regular)?
- Are any of the P waves in Figure-2 being conducted to the ventricles?
MY Thoughts:
We have already established that the QRS complex is narrow — which tells us that the rhythm in Figure-2 is supraventricular.
- Definite evidence for regular sinus P waves is seen under all RED arrows in Figure-2. The exceptions for where sinus P waves are less obvious are highlighted by the 3 PINK arrows.
- Reasons why I believe these 3 PINK arrows in Figure-2 also indicate where sinus P waves are falling are: i) The PINK arrow coinciding with the QRS of beat #7 highlights a downward deflection in the terminal portion of this QRS that is not seen in any other QRS complex; ii) The T wave of beat #8 is "fatter"-at-its-peak than any other T wave in this tracing (and — in simultaneously-occurring leads V2 and V3, there is "telltale" notching of the ST segment of beat #8); iii) There is subtle-but-real initial slurring of the QRS of beat #14 that is not seen for any other QRS complex in this long lead II rhythm strip; and, iv) Using calipers allows us to walk out a fairly (albeit not completely) regular P wave rhythm for each of the arrows in the long lead II that is consistent with sinus arrhythmia. Postulating an underlying sinus mechanism with no more than slight irregularity is far more common (and far more logical) than having to postulate sudden loss of sinus P waves.
PEARL #2: It may sometimes be extremely challenging to try and figure out if certain P waves on a tracing are (or are not) being conducted to the ventricles. In such cases — Start with what you know!
- What We Know — is that the P wave that coincides with beat #7 can't be conducting — because it begins afterthis QRS complex.
- We Also Know — that the PR intervals preceding beats #6, 13 and 14 are clearly too short to conduct.
- Considering the PR intervals preceding beats #2, 3; and 10, 11 — it would seem that the PR intervals preceding beats #4 and 12 are probably also too short to conduct. Therefore — Many (if not the majority) of P waves in the long lead II rhythm strip in Figure-2 are probably not being conducted to the ventricles!
=======================================
NOTE: I've devoted ECG Media Pearl #61 (above) to addressing the challenge for determining IF a given on-time P wave is (or is not) being conducted to the ventricles.
=======================================
PEARL #3: One of the BEST clues that one-or-more on-time sinus P waves is being conducted to the ventricles — is IF you see one-or-more QRS complexes occurring earlier-than-expected considering regularity of the R-R interval for other beats in the tracing.
- To better assess which beat(s) in Figure-2 are likely to be conducted — I carefully measured all R-R intervals in the long lead II rhythm strip (Figure-3).
 |
| Figure-3: I have measured all R-R intervals (in milliseconds) in Figure-2. Note that all but 2 of these R-R intervals are identical (See text). |
MY Thoughts on the Rhythm in Figure-3:
As I've already alluded to — the rhythm in today's case is more complex than I initially thought. Precise measurement of all R-R intervals in the long lead II rhythm strip suggests the following:
- All R-R intervals are identical (ie, measuring 720 msec.) — except for the 2 R-R intervals between beats #8-9 and 9-10 (which measure 600 and 700 msec., respectively).
- The PR interval preceding each of the 14 beats on this tracing is continually changing. But rather than progressive increase in the PR interval (until a beat is dropped) — the PR interval is decreasing as one moves from beat #2 until beat #6 — and then again as one moves from beat #9 until beat #14. This tells us that P waves are not related to neighboring QRS complexes for those beats in which the R-R interval is regular (ie, there is AV dissociation for all beats preceded by a PR interval = 720 msec.).
- Since the QRS complex is narrow and the R-R interval is perfectly regular for all but 2 beats on this tracing, during which time there is AV dissociation — this means that the rhythm for most of this tracing is junctional! It also means that there is AV dissociation for most of this tracing!
- An R-R interval of 720 msec. (ie, 3.6 large boxes) corresponds to a ventricular rate of ~85/minute. Since the usual rate of an AV nodal escape pacemaker in adults is between 40-60/minute — this defines the underlying rhythm in Figure-3 as an accelerated junctional rhythm.
QUESTION:
- WHY is the R-R interval between beats #8-9 so much shorter than all other R-R intervals in this tracing?
ANSWER:
The only logical conclusion to draw from the finding that the R-R interval between beats #8-9 is so much shorter than all other R-R intervals — is that beat #9 must be conducted!
- This means that the on-time P wave that is hiding within the T wave of beat #8 must be conducting to the ventricles with a long PR interval.
- I strongly suspect that the reason the R-R interval between beats #9-10 is also shorter (at 700 msec.) than all other R-R intervals (which are all 720 msec.) — is that beat #10 is probably also being conducted to the ventricles.
PEARL #4: Support that not only beat #9 — but also beat #10 are both conducted to the ventricles is forthcoming from a look at simultaneously-recorded leads V2 and V3. Note that although the QRS complex for beats #8, 9 and 10 in these 2 leads is narrow — QRS morphology for the 2 beats that occur earlier-than-expected (ie, beats #9 and 10) is different than for beat #8 which is on-time (ie, preceded by an R-R interval = 720 msec.).
- Because the site within the AV node from which a junctional escape beat may arise can be slightly different than the site in the AV node that a normal, sinus-conducted beat passes through — sometimes (not always!) you may see slightly different QRS morphology for junctional beats compared to sinus-conducted beats. When this finding occurs (as it does for beats #8, 9 and 10 in leads V2 and V3) — it can be very helpful in telling you whether a certain beat is or is not conducted.
PEARL #5: Despite the fact that there is AV dissociation for most of today's tracing — there is no evidence of 2nd or 3rd-degree AV block! This is because we have not proven that P waves (RED arrows) in Figure-3 had an adequate chance to conduct, but still failed to do so.
- On the contrary — 2 QRS complexes in Figure-3 are conducted (ie, beats #9 and 10) — and beat #10 is conducted with no more than minimal prolongation of the PR interval.
==========================
SUMMARY Thus Far of Today's Rhythm: This leaves us with the following conclusions about the rhythm in today's case:
- There is an underlying sinus arrhythmia (RED arrows) — with AV dissociation for most of the long lead II rhythm strip in Figure-3.
- An accelerated junctional rhythm at ~85/minute is present for most of this tracing.
- The accelerated junctional rhythm is interrupted by sinus capture of beats #9 and 10.
==========================
PEARL #6: As emphasized in ECG Blog #192 (and also in ECG Blog #191) — AV dissociation is not a diagnosis. Instead — AV Dissociation is an ECG finding that is the result of one of 3 Causes. These are: i) 2nd- or 3rd-degree AV Block (in which one or more P waves that should conduct do not conduct because of AV block); ii) AV dissociation by "Usurpation" (in which an accelerated junctional rhythm takesover the pacemaking function); and/or, iii) AV dissociation by "Default" (in which slowing = "default" of the SA nodal pacemaker allows a junctional escape pacemaker to emerge).
- As stated in Pearl #5 — there is no evidence of 2nd or 3rd-degree AV block in today's tracing. Instead — when given a "chance" to conduct — beat #10 is conducted with an almost normal PR interval.
- The cause of AV dissociation in Figure-3 is also not the result of "default" — since although the rate of sinus P waves is slower than the junctional rate — the sinus rate does not drop below 60/minute.
- By the process of elimination — the cause of AV dissociation in Figure-3 is "Usurpation" of the underlying sinus arrhythmia by an accelerated junctional rhythm, which at ~85/minute is clearly faster than the usual 40-60/minute AV nodal escape rate.
- Technically — I would interpret the ECG in Figure-3 as showing: i) An accelerated junctional rhythm at ~85/minute — which results in AV dissociation by "usurpation" over the underlying slower sinus arrhythmia; and, ii) An otherwise unremarkable 12-lead ECG with an isolated Q wave in lead III (with a tiny q in aVF) — but no acute ST-T wave changes.
PEARL #7: Did YOU notice that there is a technical mishap with lead V5, which is clearly misplaced (ie, It makes no physiologic for the QRS complex to be predominantly negative in lead V5 — when it is entirely positive in neighboring leads V4 and V6). That said — this technical mishap does not negate our overall interpretation of an unremarkable ECG except for the rhythm.
==========================
CLINICALLY: What To Do? We are told that the ECG in Figure-3 was obtained as part of a routine exam of an otherwise healthy and asymptomatic 30-year old man.
- Intermittent appearance in an otherwise healthy, young adult of a junctional escape rhythm that falls within the usual "escape range" for adults (of between ~40-60/minute) — is not unusual, and often reflects a normal variant rhythm.
- In contrast — an accelerated junctional rhythm (or junctional tachycardia) is not a common rhythm, and especially in older adults is likely the result of some underlying pathology. Among common causes of an accelerated junctional rhythm include acute ischemia/infarction — myocarditis — post-operative state — digoxin toxicity — sympathomimetic medication — shock — among other causes.
- That said — IF the patient in today's case is truly an otherwise healthy adult who is completely asymptomatic, is not abusing medication, and who has no evidence of underlying heart disease (ie, if his Echo is normal) — then it is likely that the accelerated junctional rhythm and resultant AV dissociation in Figure-3 is benign.
==========================
LADDERGRAM: For clarity of my above discussion — I propose the laddergram shown in Figure-4.
- I welcome other proposals for the mechanism of today's interesting rhythm!
 |
Figure-4: My proposed laddergram for the rhythm in today's case. Fortuitous occurrence of the on-time P wave that peaks the T wave of beat #8 allows conduction to the ventricles of beat #9, albeit with a prolonged PR interval.
==================================
Acknowledgment: My appreciation to Muhammad Zeb (from Karachi, Pakistan) for allowing me to use this case and these tracings.
==================================
Related ECG Blog Posts to Today’s Case:
- ECG Blog #205 — Reviews my Systematic Approach to 12-lead ECG Interpretation.
- ECG Blog #185 — Reviews my Systematic Approach to Rhythm Interpretation.
- ECG Blog #192 — Reviews the 3 Causes of AV Dissociation — and emphasizes why AV Dissociation is not the same thing as Complete AV Block.
- ECG Blog #191 — Emphasizes the difference between AV Dissociation vs Complete AV Block.
- I believe Dave's scenario is valid. I had made similar observations that he describes — but I had decided not to mention these for 3 reasons: i) I didn't want to further complicate my already complicated explanation; ii) We can not fully see the T wave that precedes beat #1 (so hard to tell if a P wave is hidden within); and, iii) In the other simultaneously-obtained 11 leads (above the long lead II rhythm strip) — I thought there was some variation in QRST morphology that was not totally consistent ...
- BOTTOM LINE: Dave's theory is equally valid as mine. I believe we both agree that there is AV dissociation by "usurpation", resulting from an accelerated lower pacemaker (which could indeed cause "fusion" beats if originating from within the conduction system [ie, the His] but below the AV Node). I do not think it possible to know for certain what the true mechanism of this arrhythmia is from this single tracing. We both agree that the mechanism is more complex than one might initially think. Regardless of the fascinating details of whatever the true mechanism is — I think the cliical approach I suggested above remains valid.
You rightly point out that beats 9 and 10 have a slightly different QRS shape from that of the rest of the beats because they are conducted beats. This is evident not only from the QRS shape in leads V2 and V3, but also from a slightly narrower QRS in lead II. Technically the QRS width is similar at the base of the complex, but the R wave narrows as it rises in the conducted beats, resulting in them occupying a smaller area. However, although beat 10 has a narrower-than-usual QRS, it’s not as narrow as that of beat 9. In V2 and V3 beat 10 also has an S wave depth and T wave height that are intermediate between those of beats 8 and 9. Therefore, I think beat 10 may be a fusion beat – partly conducted via the normal AV-node-His pathway, and partly via the slightly different conduction route of the junctional escape beats. I admit that I don’t what the anatomical basis of this slightly different conduction route might be.
Knowing that the conducted beats have a slightly different QRS morphology from the escape beats in lead II — I re-examined the rest of the ECG to see if there might be evidence of additional conducted or fusion beats. It appears that beats 1 and 2 also have slightly narrower complexes in lead II, and a deeper S wave in lead I — so perhaps they too are conducted or, perhaps more likely, fusion beats, with each showing a different degree of fusion as evidenced by the different S wave depths in lead I. Certainly, there is no reason to think that the P wave before beat 2 should not be able to conduct and its PR interval is very similar to that of beat 10.
This ECG may be even more complex than it first appears! — Dave
 |
| Figure-5: I've added YELLOW arrows to today's tracing to highlight those P waves that David Richley feels may be conducting (I drew this figure to illustrate Dave's comment above). |


What about the strange V5?
ReplyDeletePlease see my Pearl #7 above — which emphasizes that some type of technical mishap (lead misplacement) HAS TO BE the reason for the unexpected all negative appearance of the QRS in lead V5 — :)
Delete