The ECG shown in Figure-1 was obtained from a middle-aged woman being treated for an acute exacerbation of her asthma. This tachycardia developed after a series of nebulizer treatments. The patient was short of breath from her asthma — but hemodynamically stable.
- What is the rhythm?
- Where are the P waves? (Are P waves present before or after the QRS? — or are there no P waves at all?).
 |
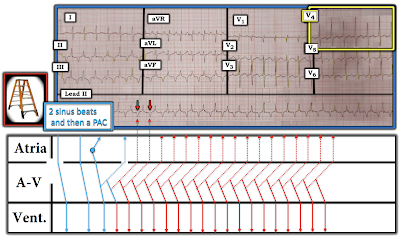
| Figure-1: ECG obtained from a middle-aged woman being treated with nebulizers for an exacerbation of asthma. |
=======================================
NOTE: Some readers may prefer at this point to listen to the 7:30 minute ECG Audio PEARL before reading My Thoughts regarding the ECG in Figure-1. Feel free at any time to refer to My Thoughts on this tracing (that appear below ECG MP-83).
=======================================
Today’s ECG Media PEARL #83 (7:30 minutes Audio) — Reviews the ECG finding of Electrical Alternans (See ECG Blog #83 — for more on this subject).
My Approach to Today's Case:
Since the patient was hemodynamically stable — there was time for systematic assessment of the rhythm. By the Ps, Qs, 3R Approach (See ECG Blog #185):
- The rhythm is fast and Regular. I estimate the ventricular Rate to be ~160/minute (ie, the R-R interval is just under 2 large boxes in duration).
- The QRS is narrow (ie, clearly not more than half a large box in duration) — which means that the rhythm is supraventricular.
- Sinus P waves are absent — because there is no consistent upright deflection (P wave) before the QRS complex in lead II. Instead, it looks as there is negative atrial activity in at least a number of leads (BLUE arrows in each of the inferior leads in Figure-2). The timing of these negative inferior lead deflections corresponds to the positive pointed deflection (BLUE arrow) in lead aVR.
PEARL #1: The question arises as to whether the deflections highlighted by BLUE arrows in Figure-2 are truly P waves — and if so, whether these are retrograde P waves occurring after the QRS complex — or — negative P waves preceding the next QRS complex? All 3 of these possibilities should be considered. That said — reasons why I strongly suspected these deflections represented retrograde P waves with a long RP' interval (ie, long distance from the preceding QRS complex) were the following:
- These deflections "look" much more like retrograde P waves.
- The deepest point of these deflections in the inferior leads (and the tallest point in lead aVR) are much more pointed than one usually sees in a T wave.
- The PR interval if anything, shortens with tachycardia. IF these deflections were forward-conducting — then the PR interval would be longer-than-expected given the tachycardia.
- IF the rhythm was an ectopic ATach (Atrial Tachycardia) — then we'd have to postulate a huge negative P wave! (which is possible, but less likely).
- On the other hand — both the location of these deflections and their morphologic appearance is perfectly consistent with the "Fast-Slow" form of AVNRT (See Figures-5 and -6 in ECG Blog #240).
- Further support in favor of this rhythm being a reentry SVT (in this case, of the "Fast-Slow" form of AVNRT) — is forthcoming from from the presence of Electrical Alternans in Figure-2 (best seen in lead V4 — in which QRS amplitude varies every-other-beat).
 |
| Figure-2: I've labeled with BLUE arrows the deflections from Figure-1 that I strongly suspect represent retrograde P waves with a long RP' interval (See text). |
PEARL #2: The subject of today's Audio Pearl (ECG-MP-83 — See above) is Electrical Alternans — with more detailed discussion on this ECG phenomenon found in ECG Blog #83.
- Although there are many potential causes of Electrical Alternans — when seen in a patient with a regular SVT rhythm, this ECG finding strongly suggests a reentry mechanism (either with participation of an Accessory Pathway — or with the reentry circuit entirely contained within the AV Node).
- Although usually seen in several leads — Electrical Alternans may only be seen in a single lead. There should be no mistaking the every-other-beat alternation of QRS amplitude in lead V4 (Look within the YELLOW rectangle in Figure-3).
- Alternation of one or more parts of the QRST complex is most often seen every-other-beat — but can occur at other frequencies. As a result — I interpreted the variation in QRS appearance that we see in the long lead II rhythm strip as also consistent with Electrical Alternans. This finding essentially rules out the possibility that the negative inferior lead deflections are forward-conducting P waves from an Atrial Tachycardia — because ATach is an "automatic" tachycardia, and not subject to AV nodal reentry (and therefore far less likely to produce Electrical Alternans).
The Mechanism of the "Fast-Slow" Form of AVNRT:
The various types of reentry SVT rhythms were discussed and illustrated in ECG Blog #240. In brief — for those reentry SVT rhythms in which the reentry circuit is entirely contained within the AV Node (ie, AVNRT = AtrioVentricular Nodal Reentry Tachycardia) — most of the time, the electrical impulse travels first down the slower AV Nodal pathway — which means that the reentry circuit back to the atria is conducted over the faster AV Nodal pathway (ie, the much more common "Slow-Fast" form of AVNRT).
- Since retrograde conduction back to the atria is over the "faster" AV Nodal pathway — this most common "Slow-Fast" form of AVNRT will manifest retrograde P waves with a very short RP' interval (in which the retrograde P wave will either be hidden within the QRS complex — or occur immediately after the QRS).
- In contrast, with the far less common "Fast-Slow" form of AVNRT — retrograde conduction will be over the "slower" AV Nodal pathway — which will result in retrograde P waves with a much longer RP' interval (as seen in Figure-3 in today's case).
PEARL #3: The KEY clue for determining the etiology of an SVT rhythm often lies with capturing either the beginning and/or the end of the SVT rhythm.
- ATach often begins gradually — with progressive acceleration of the ectopic atrial focus (ie, "warm-up" phenomenon). There may then be gradual slowing of the ectopic atrial focus (ie, "cool-down") as the tachycardia ends.
- In contrast — SVT reentry rhythms often start with 1 or more PACs, that because of their early arrival at the AV node — encounter a block in conduction down one of the AV Nodal pathways that is still in its refractory state. This block in conduction down one of the AV Nodal pathways sets up the conditions that enable a reentry circuit to form, as the impulse is diverted and starts down the other pathway.
- The onset of a reentry SVT is often abrupt (ie, accounting for the previous term used to designate this rhythm = PSVT = Paroxysmal SVT). The termination of reentry SVT rhythms is also usually quick (though termination may occur over a period of several beats).
The Laddergram in Figure-3:
We failed to capture the onset of the SVT rhythm in today's case. That said, for illustrative purposes — I've drawn in BLUE in the Figure-3 Laddergram the theoretical sequence of events that usually precedes (initiates) a reentry SVT rhythm.
- For illustrative purposes — I began the laddergram in Figure-3 with 2 normal sinus beats (BLUE lines passing normally through the Atrial, AV Nodal and then Ventricular Tier).
- After 2 normal sinus beats — I next drew a PAC (small BLUE circle with its origin in the middle of the Atrial Tier). This PAC conducts both back to the atria — and forward to the ventricles.
- IF conditions are "just right" — this PAC may find one of the AV Nodal pathways able to conduct retrograde back to the atrial (dotted BLUE lines).
- IF conditions continue to be "just right" — the impulse from this retrograde conduction may "turn around" and conduct back down toward the ventricles. If these "just right" conditions are maintained — this may initiate a self-sustaining reentry circuit (schematically illustrated by solid and dotted RED lines for the rest of the tracing).
- Depending on whether the PAC that initiated this reentry circuit traveled first down the "Fast" or the "Slow" AV Nodal pathway — will determine whether the mechanism of this AVNRT rhythm is of the more common "Slow-Fast" type — or the less common "Fast-Slow" type seen in today's case (and illustrated in this Figure-3 laddergram).
The CASE Continues:
The patient was treated with IV Verapamil. Serum K+ was found to be low — and was replaced. The 2 non-consecutive long lead II rhythm strips shown in Figure-4 show the result of this treatment.
- Describe the effect of the above treatment.
- Look again! What happens to the RP' interval during the course of treatment?
ANSWER:
The end result of the above treatment was conversion to sinus rhythm — which occurred just after beat #10 in Tracing B. Of interest are the subtle changes that occur in the rhythm during the conversion process:
- Although difficult to appreciate unless you measure with calipers — there is slight variation in the R-R interval in both tracings until conversion to sinus rhythm.
- Attention to the T waves in both tracings until conversion to sinus rhythm — shows beat-to-beat variation in T wave morphology. I believe the reason for this is ongoing variation in the RP' interval produced by the IV Verapamil that is altering retrograde conduction properties within the AV Node.
- Probably contributing to this beat-to-beat variation in QRST morphology is the phenomenon of Electrical Alternans.
A Final Laddergram:
Confirmation of AV Nodal reentry as the mechanism for the SVT in today's case is shown in Figure-5:
- The first 9 beats in Tracing B show continuation of the reentry SVT rhythm — albeit with the slight variation in R-R interval plus the ongoing change in T wave morphology described above.
- Note that there is no indication of any retrograde P wave following beat #10. This is shown schematically in the laddergram with a dotted line ending in a terminal butt end before making it through the Atrial Tier.
- This failure to produce a retrograde P wave after beat #10 allows the SA Node a moment to recover — which results in conversion to sinus rhythm beginning with beat #11.
Final PEARL #4: While our goal is always to arrive at as precise of a rhythm diagnosis as possible — the "good news" regarding treatment of an undifferentiated regular SVT — is that for practical purposes, initial diagnostic and/or treatment measures in the field or in the ED are similar (ie, consideration of a vagal maneuver — and/or use of an AV nodal blocking agent such as Verapamil/Diltiazem; a ß-Blocker and/or Adenosine if available).
- Most of the time — one or more of these initial treatment measures will either be successful — or — will allow a more definitive diagnosis to be made, that enables a more targeted treatment.
- NOTE: Reentry SVT rhythms have a tendency to recur if conditions predisposing to their onset are not addressed. As a result — Be aware that there will often be a need to initiate longer-duration therapy after initial conversion to sinus rhythm (either by IV infusion or by addition of oral antiarrhythmic therapy).
=======================
Acknowledgment: My appreciation to Kenneth Khoo (from Malaysia) for the case and this tracing.
=======================
=============================
Relevant LINKS to Today's Case:
=============================
Additional Relevant Material to Today's Case:
- See ECG Blog #185 — for review of the Systematic Ps, Qs, 3R Approach to rhythm interpretation.
- See ECG Blog #83 — for more on Electrical Alternans.
- See ECG Blog #263 — for another case of Electrical Alternans.
- See ECG Blog #240 — for Review on the ECG assessment of the patient with a regular SVT rhythm (including distinction between the various types of SVT reentry).
How to Draw a Laddergram (Step-by-Step Demonstration)
- See ECG Blog #69 — for a Step-by-Step description on drawing a Laddergram.
- See ECG Blog #188 — for a brief ECG Video review on the basics of what a Laddergram is — with LINKS at the bottom of the page to more than 50 ECG blog posts in which I review illustrative laddergrams.
- See ECG Blog #164 — for a user-friendly rhythm-solving approach to AV Wenckebach, followed by Step-by-Step construction of the Laddergram.
- CLICK HERE — to DOWNLOAD my Free PowerPoint Laddergram STENCIL for your use as desired.
===================================
ADDENDUM (2/6/2022):
I thought it important to add the comment I received from Nestor Rodrigues de Oliveira Neto regarding this case. Nestor wrote the following:
- "Another possibility here is Permanent Reciprocal Junctional Tachycardia (also known as Coumel Tachycardia) — which is a rare form of supraventricuar tachycardia that is usually incessant, and characterized by retrograde conduction via an AP (Accessory Pathway). Although more common in children and young adults — in cases of Coumel's Tachycardia, the P waves have a morphology similar to the one presented in today's ECG Blog #281.
My Answer:
- Thank you Nestor. I completely agree with you! Here is a nice case study by Valiente et al (Anales de Pediatría 87(3): 173, 2017) — in which Figure-1 in their article looks virtually the same as Figure-1 in today's ECG Blog #281.




Congratulations, dear Dr. Ken Grauer,
ReplyDeleteyour ECG discussions are always very interesting, I am a reader of his blog.
One possibility here is permanent reciprocal junctional tachycardia, also known as Coumel tachycardia, which is a rare form of supraventricular tachycardia that is usually incessant, characterized by retrograde conduction via an accessory pathway.
Although more common in children and young adults, in cases of Coumel's tachycardia the P waves have a morphology similar to the one presented.
Thanks!
Nestor Rodrigues
Muito obrigado por seu comentário, Nestor. Concordo plenamente com você! (Many thanks for your comment Nestor — I completely agree with you!). Here is a nice case study by Valiente et al (Anales de Pediatría 87(3): 173, 2017) — with the ECG in Figure-1 looking the SAME as the one in my case! Here is the LINK — tinyurl.com/KG-Coumel-Tachycardia — :)
DeleteNestor — I thought your comment important — and have just now added it as an Addendum to today's post (with acknowledgment to you). THANK YOU again! — :)
Delete