- How would YOU interpret this ECG?
- What treatment(s) would you consider?
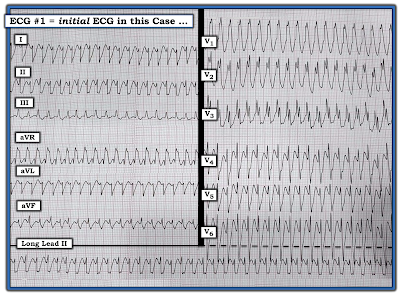 |
| Figure-1: This ECG is from a 40-year old woman with chest pain. What is the most likely cause of this WCT rhythm? |
- At this point — it matters less what the rhythm in Figure-1 is, since IF this patient is "hemodynamically unstable" — then regardless of whether the rhythm is VT (Ventricular Tachycardia) — or — an SVT (SupraVentricular Tachycardia) with either preexisting BBB (Bundle Branch Block) or aberrant conduction — the immediate treatment of choice is electricity (ie, synchronized cardioversion).
- On the other hand — IF despite the tachycardia, the patient is stable and tolerating the arrhythmia — then by definition, we have at least a moment in time to better assess the rhythm and contemplate therapeutic options.
- In today's case — a close "look" at the patient would be our 1st Priority — since we need to determine IF symptoms (ie, the patient's chest pain) in association with the fast heart rate on this ECG — are enough to mandate immediate cardioversion. (For more on determining Hemodynamic Stability — See ECG Blog #220 — including the Audio Pearl in this post).
- To emphasize — You do not have to go in sequence when applying the Ps, Qs, 3Rs approach. The point of this memory aid is simply to recall the 5 parameters that need to be assessed in whatever sequence seems best to you for the case at hand.
- In today's case — I looked first at QRS width. That the QRS is wide — is immediately evident from the appearance of the complexes in leads V1, V2 and V3.
- The rhythm in Figure-1 is fast and Regular. As shown in the blow-up of leads I and II from today's tracing (Figure-2) — I estimate the Rate of the rhythm to be just under 250/minute.
 |
| Figure-2: Application of the "Every-Other-Beat" Method for rapid estimation of heart rate in today's case. Looking at every-fifth-beat is easiest in this tracing — because I found a 5-beat period in the rhythm in which a part of the QRS at the beginning and at the end falls either on (or almost on) a heavy grid line (as per the 2 vertical RED lines in this Figure). The amount of time that it takes to record 5 beats (RED numbers in lead I) is just over 6 large boxes (BLUE numbers in this Figure). Therefore — ONE FIFTH the rate is a little less than 300/6 ~49/minute — which means that the actual rate for the rhythm in Figure-1 is ~49 X 5 or ~245/minute. (For more on the Every-Other-Beat Method — See ECG Blog #210). |
- No P waves are seen in Figure-1. This of course means that there is no Relation between P waves and the QRS.
- Statistically — the odds that a regular WCT rhythm without clear sign of atrial activity will turn out to be VT are at least 80%. As a result — we need to prove that a rhythm is not VT, rather than the other way around.
- Assessment of QRS morphology can help to increase or decrease the statistical likelihood of our diagnosis. As discussed in ECG Blog #211 — the finding of QRS morphology typical for RBBB conduction favors a supraventricular etiology. This entails: i) An rSR' complex in lead V1, in which the S wave descends below the baseline — and in which there is a thin and taller "right rabbit ear" (ie, the R' is taller than the initial r wave); and, ii) The finding of wide, terminal S waves in lateral leads I and V6.
- Completely typical QRS morphology for other forms of known conduction defects (ie, LAHB, LPHB, LBBB) will also favor a supraventricular etiology (See ECG Blog #203 and Blog #204 — for review of expected morphology for the hemiblocks and BBBs).
- No set of morphologic criteria is perfect for distinguishing between VT vs SVT with preexisting BBB or aberrant conduction. There are always exceptions (ie, patients with severe underlying heart disease who have extremely unusual QRS morphology on their baseline tracing when in sinus rhythm). Nevertheless, as a general rule — QRS morphology consistent with a typical appearance of some known form of conduction defect favors a supraventricular etiology. In contrast — an "uglier" QRS morphology that does not resemble any known form of conduction defect will favor VT.
- Finding a baseline ECG on the patient can help — by showing you what QRS morphology normally looks like in sinus rhythm. IF this QRS morphology during sinus rhythm is identical in virtually all leads to the QRS morphology during the WCT rhythm — this strongly supports a supraventricular etiology.
- To emphasize — Whereas a completely typical QRS morphology for a known form of conduction defect supports a supraventricular etiology — the opposite is not necessarily true. This is because QRS morphology will sometimes be atypical with BBB or aberrant conduction. Attention to other features will then be needed.
- Among the most helpful features in my experience for predicting VT — is the presence of extreme axis deviation. By this I mean that the QRS is entirely negative in either lead I or in lead aVF. However, if there is any positivity (ie, such as the small-but-definitely-present initial r wave in lead I of Figure-1) — then this criterion does not apply (See ECG Blog #220 for additional criteria to distinguish between VT vs SVT).
- Finally — IF at all in doubt about the etiology of a regular WCT rhythm without atrial activity — Assume VT. Remember — We need to prove that a rhythm is not VT, rather than the other way around.
What about QRS Morphology in Figure-1?
Remember — Since the rhythm in Figure-1 is a regular WCT without clear sign of atrial activity — statistical odds that this rhythm is VT are ~80% even before we begin to look at QRS morphology.
- In Figure-1 — QRS morphology superficially resembles RBBB with a hemiblock. That said — there are several atypical morphologic features that I believe strongly favor the diagnosis of Fascicular VT.
- Although the QRS is all upright in lead V1, and manifests wide terminal S waves in lateral leads I and V6 — the QRS in lead V1 is unformed, in that it lacks a clear triphasic (rSR') pattern with an S wave that descends below the baseline — and it lacks a clean, tall and thin terminal "right rabbit ear".
- Although the deep descent of the S wave in lead I is typical for LPHB — the QRS should be predominantly positive in both leads II and III with this conduction defect (and not predominantly negative in lead II as seen in Figure-1).
- Although the predominantly negative QRS in lead II of Figure-1 is typical for LAHB — a similar predominantly negative QRS should also be seen in lead III with this conduction defect. In addition — the QRS should be predominantly positive in lead I when there is LAHB.
- BOTTOM LINE: QRS morphology in Figure-1 is distinctly atypical for any known form of conduction defect. This increases the odds from ~80%, to over 90% that this rhythm is VT.
Do Previously Healthy Young Adults get VT?
Approximately 10% of patients who present with VT do not have ischemic or underlying structural heart disease. The importance of recognizing these patients with Idiopathic VT who have a structurally normal heart — is that the presentation, clinical course, and both short- and long-term management differ greatly compared to the ~90% of patients with the "usual" ischemic or structural forms of VT (See Figure-3 below in the ADDENDUM — for a Summary on the Idiopathic VTs).
- The "good news" regarding patients who present with idiopathic VT — is that long-term prognosis of these patients tends to be surprisingly good (and much better than the usual prognosis of patients who present with frequent runs of ischemic VT).
- The fact that the patient in today's case was a previously healthy 40-year old woman is consistent with the most common patient profile of idiopathic VT — in that younger adults without prior heart disease are most often affected.
- In today's case — it is the partial resemblance to RBBB with hemiblock in this previously healthy 40-year old woman, that strongly suggested the diagnosis of Fascicular VT to me — so much so that I would have tried IV Verapamil as an initial therapy (See ECG Blog #197 — for more on the Idiopathic VTs).
P.S. (Beyond the Core) — There is a final possibility for the etiology of the rhythm in Figure-1. In addition to VT or SVT with either preexisting BBB or aberrant conduction — the etiology of this regular WCT rhythm could be the reentry SVT rhythm known as AVRT (AtrioVentricular Reciprocating Tachycardia) — in which an AP (Accessory Pathway) participates in the reentry circuit.
- Depending on the initial direction of the impulse during the reentry tachycardia — AVRT will either be orthodromic or antidromic (ie, going initially down the AV node — or going initially down the AP).
- Over 95% of AVRT rhythms are orthodromic (ie, traveling first down the normal AV nodal pathway — and then back to the atria by retrograde conduction over the AP). As a result — over 95% of AVRT rhythms will manifest a narrow QRS complex.
- In those rare (~5%) instances in which AVRT is antidromic — the QRS complex will be wide (because the impulse bypasses the AV node — and travels first down the AP). In such cases — the AVRT rhythm may be indistinguishable from VT. It may only be after conversion to sinus rhythm that "telltale" delta waves of WPW can be identified.
- Since AVRT is a supraventricular rhythm that utilizes the AV node as part of its reentry circuit — both orthodromic and antidromic forms of AVRT may respond to Adenosine, Verapamil/Diltiazem and/or Beta-Blockers (See ECG Blog #18 — for more on the types of arrhythmias seen in patients with WPW).
- Because antidromic AVRT is so uncommon — we often don't think of it when formulating our differential diagnosis of the regular WCT rhythm. That said — it's good to be aware that this uncommon rhythm is a possibility (as it may explain some of the instances in which Adenosine or other AV nodal blocking agents are successful in converting an occasional WCT rhythm).
- Finally, in Figure-1 — the exceedingly rapid rate of this WCT rhythm (ie, ~245/minute) does raise the possibility that rather than Fascicular VT — the etiology of this rhythm could be antidromic AVRT in a patient with WPW. Unfortunately — I do not have follow-up for this case. That said, regardless of whether the etiology of this rhythm was VT or AVRT — the fact that this patient was symptomatic with this WCT rhythm at such a fast rate of itself is indication for EP referral.
==================================
Acknowledgment: My appreciation to Rasha M. Khalid (from Babil, Iraq) for the case and this tracing.
==================================
- ECG Blog #205 — Reviews my Systematic Approach to 12-lead ECG Interpretation.
- ECG Blog #185 — Reviews my System for Rhythm Interpretation, using the Ps, Qs & 3R Approach.
- ECG Blog #210 — Reviews the Every-Other-Beat Method for estimation of fast heart rates — and discusses another case of a reguar WCT Rhythm.
- ECG Blog #203 — Reviews the expected QRS morphology for the Hemiblocks and Bifascicular Blocks (ie, LAHB, LPHB; RBBB/LAHB; RBBB/LPHB).
- ECG Blog #204 — Reviews the expected QRS morphology for the Bundle Branch Blocks (ie, RBBB, LBBB, IVCD).
- ECG Blog #211 — Reviews why Aberrant Conduction occurs (with illustration of those QRS morphologic features that predict aberrant conduction).
- ECG Blog #196 — Reviews another Case of a Regular WCT Rhythm.
- ECG Blog #197 — What is Idiopathic VT? — WHY do we care? Special attention to the 2 most common forms = RVOT VT and Fascicular VT.
- ECG Blog #220 — Case Study that reviews criteria for Distinction beween VT vs SVT with preexisting BBB or aberrant conduction (including Audio Pearl MP-37 — Is the Patient Hemodynamically Stable?).
- ECG Blog #38 and Blog #85 — Review of Fascicular VT.
- ECG Blog #35 — Review of RVOT VT.
- ECG Blog #42 — Comprehensive review of criteria for distinguishing VT vs Aberration.


Excellent explanation. One question. Looking at V6, the complex is not entirely negative which may not support VT. Is there a reason for this?
ReplyDeleteGracias.
When assessing a regular WCT rhythm — IF the QRS is all negative in lead V6 — then this strongly suggests VT. But the opposite is NOT true. Lead V6 is ONLY of help from a morphologic standpoint IF the QRS is all negative (or almost all negative) — but otherwise, if there is an r wave more than 1-2 mm, this is of NO help in distinguishing between SVT vs VT.
DeleteThank you so much for the amazing explanation!
ReplyDeleteA question please, you said that both antidromic and orthodromic AVRT respond well to adenosine and verapamil/ deltiasm . But aren't those medications contraindicated in WPW? Thank you
@ Dimah — This gets challenging. Adenosine may shorten the refractory period of atrial tissue — which could initiate AFib in a predisposed individual. As a result — Adenosine should be used with caution in patients with known WPW, given theoretic possibility of inducing AFib (which could have significant consequence in a patient with accessory pathways). That said, both antidromic and orthodromic AVRT utilize the normal AV nodal pathway — so chances are that Adenosine will rapidly convert the rhythm. That said — nothing is perfect, and Adenosine can cause adverse effects in any patient who receives the drug — so IF a tachycardia results following administration, be ready to cardiovert.
DeleteCan we get pdf versions of these blog posts?
ReplyDeleteTHANKS for your comment, which I take as positive feedback! NO, there is no "direct" provision for getting PDFs of the Blog posts. That said — the material is part of the "FOAM" movement ( = Free On-Line Access Medical Education) — so you could click on the link for any blog and "Print" on your computer (will I'm afraid be a lot of pages) — OR — with a little more "work" — you could select the entire text of any blog — add in the pictures — and make your own PDFs ... To do this — you can click on the pictures and then make screen shots of them. It's a bit of a process (for someone comfortable with screen shots, and putting text + pictures into a PDF — would probably take about 10 minutes ...). As it is — I spend MANY HOURS for EACH blog that I make — so I won't be making specific PDF files (which would take me much longer to do ...) — but my material is FREE — and as long as you acknowledge me (and add a link to my blog site) — I am happy for others to use my Blog materials in anyway that they like.
DeleteNOTE: I've made "tinyurl" links for virtually all blogs. This is the formula — https://tinyurl.com/KG-Blog-XXX — in which all you need to do to get the link is replace "XXX" with the number of the blog (ie, would be https://tinyurl.com/KG-Blog-278 — for Blog #278) — so I've made it as EASY as I can for ready access ANYTIME on the internet! THANKS again for your interest! — :)